Sprained Ankle
Ankle sprains are quite common, whether young or old. Most sprains are minor and need no medical attention, but when there is intense swelling and pain, you need to seek treatment.
Depending on how much damage is done to the ligaments, some sprains can weaken the ankle to the point of arthritis, chronic ankle pain and ongoing instability.
ANATOMY
The ankle has ligaments on two sides:
- Lateral Side (outside)
- Medial Side (inside)
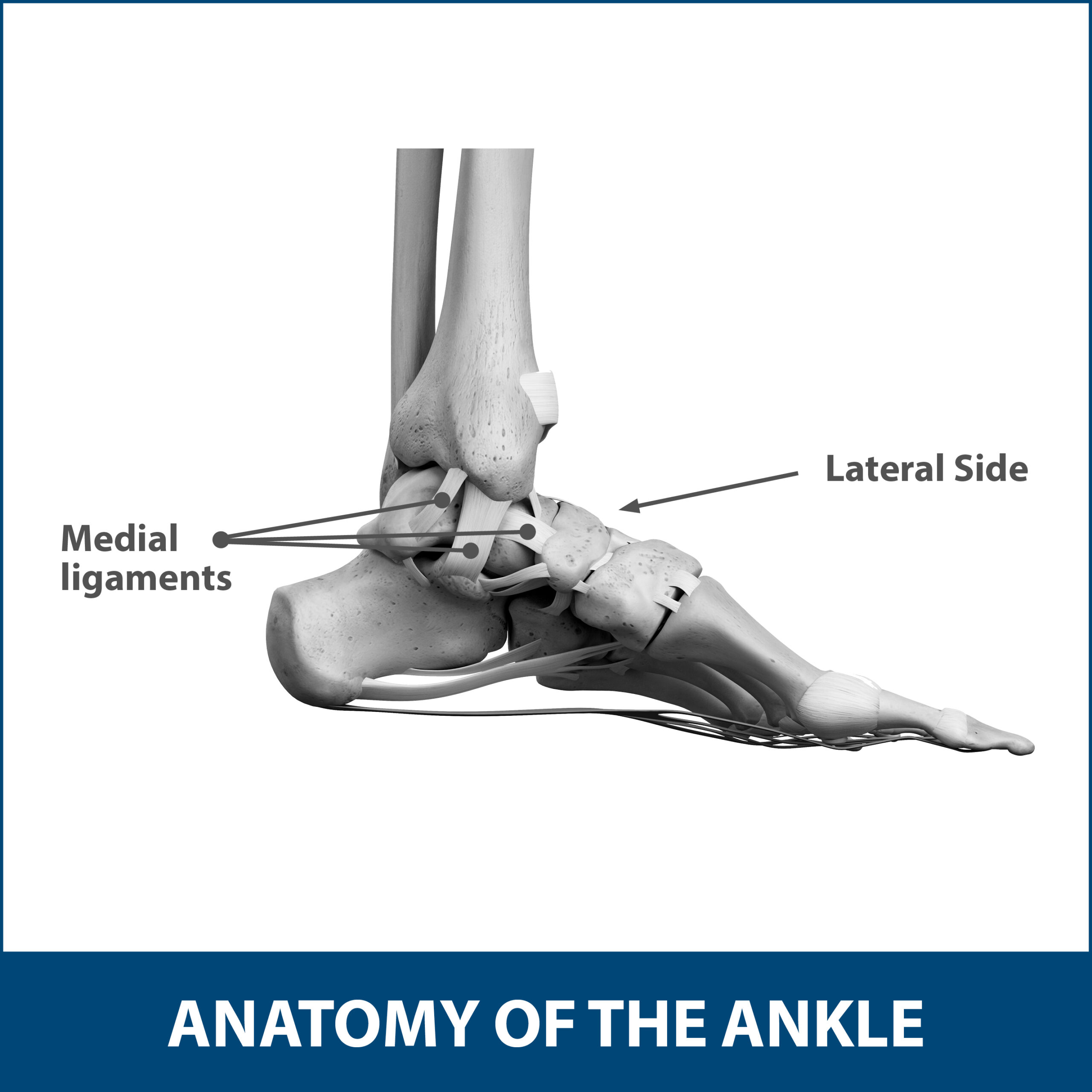
The lateral side of the foot, if looking down, is the side facing out (or the right side of your right foot and the left side of your left foot). It is home to the lateral ligaments, some of the most susceptible to tears. Most ankle sprains occur on this side.
The medial side of the foot, if looking down, is the side facing in (or left side of your right foot and right side of your left foot). It is home to the medial ligaments. Tears can occur on this side, but it is far less likely.
Ligaments are strong, fibrous tissues that connect your bones to other bones. The ligaments in your ankle do this so that the bones are held in place, and the joints are stabilized.
If there is an injury sustained to either side’s ligaments, it could create an un-stabilization of the ankle that could lead to long-term issues.
DESCRIPTION
When there is a sprain in your ankle, you technically are not “spraining” anything at all. A sprain is a tear in the ligament that can range from tiny to completely torn depending on severity.
It is not uncommon for your foot to twist unexpectedly in normal day-to-day activity. A twisting motion due to walking, engaging in sports, or falling can cause pressure on the ligaments that might create a tear.
Ankle sprains can occur in all ages and, if they happen consistently, can weaken your ability to perform activities at your body’s full potential.
SYMPTOMS
Those who experience a sprained ankle normally feel pain varying from mild to severe depending upon how intensely the ligament has been torn.

The most common symptoms of a sprained ankle are:
- Swelling
- Bruising
- Tenderness to touch
- Instability of the ankle (In severe cases, this instability could mean there has been a full tear of the ligament or complete dislocation of the joint)
If there has been a full-intensity tear, you might also hear or feel a “pop” when the sprain occurs. This is only in the most severe cases, but if this “pop” does occur, it is advised to seek immediate medical evaluation. Symptoms of this type of severe ankle sprain are like those of a broken bone.
DIAGNOSIS
During a physical examination, your Florida Orthopaedic Institute physician will ask about your symptoms and medical history. They will perform a careful examination of your foot and ankle (which may be painful depending on the severity of the sprain).
Your physician will palpate the ankle, which means they will gently press all around it to determine which ligaments are affected. They will also test for the range of motion by moving your ankle in different directions. In most cases, a sprained and swollen ankle will not have much range of motion.
If there is no broken bone, your physician will likely be able to tell the severity of the sprain due to the swelling, pain and bruising it exhibits. If this is not the case, your physician may order x-rays to ensure that a bone has not been broken as well.
Besides standard x-rays, your physician may order the following:
- Stress x-rays: Scans taken while the ankle is being moved around. They help show if the movements are abnormal.
- Magnetic resonance imaging (MRI) scans: In the most severe cases, an MRI may be ordered if your physician believes that there could be deeper damage to the ligaments and bones, or if there was a bone chip.
- Ultrasound: Scans that allow for your physician to view the stability of the affected ligaments.
After the examination, your physician will determine the grade of your ankle sprain. The grade of the sprain is determined by how much damage has been done to the ligaments.
- Grade 1 Sprain: A mild, common sprain. There may be a slight stretching and tiny tears to the ligaments along with swelling.
- Grade 2 Sprain: A moderate sprain that is accompanied by a partial tear of the ligament. There may be significant swelling and tenderness.
- Grade 3 Sprain: The most severe sprain, due to the ligament completely tearing. This is the most intense sprain, usually accompanied by intense swelling and pain.

TREATMENT FOR ANKLE SPRAINS
The good news is that almost all ankle sprains are treatable at home and without surgery. Even the most severe tears in the ligaments can be healed without any surgical repair if the ankle does not have unneeded pressure on it.
A three-phase program can help recover all ankle sprains:
- Phase 1: Resting and protecting the ankle.
- Phase 2: Restoring range of motion and strength.
- Phase 3: Slowly returning to activities that do not require turning or twisting of the ankle.
NONSURGICAL TREATMENT
The Florida Orthopaedic Institute’s philosophy is to try all appropriate nonsurgical methods first to increase mobility and function. Since most sprains of the ankle can be healed right at home, there are many nonsurgical treatment options available.
Following the RICE protocol is a good rule of thumb to heal as quickly and safely as possible.
- Rest your ankle.
- Ice the affected area to reduce swelling.
- Compression bandages will support your ankle.
- Elevate your ankle above the level of your heart as much as possible for the first 48 hours.
Medication may also be prescribed in the form of nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil, Motrin) and naproxen (Aleve). These assist with swelling and pain while you recover.
Depending on severity, walking may be initially difficult. Your Florida Orthopaedic Institute physician will determine if crutches may be necessary to assist with healing. In some cases, immobilization and physical therapy may be recommended. Strength exercises and balance training can help with improvement of range of motion.
SURGICAL TREATMENT
Most nonsurgical treatment options will help heal a sprained ankle within a few weeks. If nonsurgical treatments do not do the trick, surgical options may include:
- Arthroscopy: A small camera is used through a tiny incision in the ankle joint to direct the surgeon where loose fragments of bone or cartilage need to be removed.
- Reconstruction: The torn ligament is repaired with stitches or sutures, and the damage is replaced with tissue obtained from other ligaments and tendons found in the foot or ankle.
Most surgical procedures of the ankle require immobilization and rehabilitation of some form. The length of recovery time varies depending on injury severity and the amount of surgery done. Most rehabilitation will take anywhere from a few weeks to a few months.
THE NEXT STEP
If you have pain in your ankle, call Florida Orthopaedic Institute to schedule an appointment for an evaluation. All Florida Orthopaedic Institute surgeons are fellowship trained, adding further expertise in their specialty. They stay current on the latest ankle sprain research and treatments and will discuss all your treatment options.
Areas of Focus
- Foot, Ankle & Lower Leg
- Achilles Tendinitis - Achilles Insertional Calcific Tendinopathy (ACIT)
- Achilles Tendon Rupture
- Achilles Tendonitis
- Ankle Fracture Surgery
- Ankle Fractures (Broken Ankle)
- Ankle Fusion Surgery
- Arthroscopic Articular Cartilage Repair
- Arthroscopy Of the Ankle
- Bunions
- Charcot Joint
- Common Foot Fractures in Athletes
- Foot Stress Fractures
- Hallux Rigidus Surgery - Cheilectomy
- Hammer Toe
- High Ankle Sprain (Syndesmosis Ligament Injury)
- Intraarticular Calcaneal Fracture
- Lisfranc Injuries
- Mallet, Hammer & Claw Toes
- Metatarsalgia
- Morton’s Neuroma
- Neuromas (Foot)
- Orthopedic Physician Or A Podiatrist? Definition of a Podiatrist
- Plantar Fasciitis
- Sports Foot Injuries
- Sprained Ankle
- Total Ankle Replacement
- Turf Toe
The following Florida Orthopaedic Institute physicians specialize in Sprained Ankles:
Specialties
- AC Joint Injuries
- Achilles Tendinitis - Achilles Insertional Calcific Tendinopathy (ACIT)
- Achilles Tendon Rupture
- Achilles Tendonitis
- ACL Injuries
- Ankle Fracture Surgery
- Ankle Fractures (Broken Ankle)
- Ankle Fusion Surgery
- Anterior Cervical Corpectomy & Discectomy
- Arthroscopic Articular Cartilage Repair
- Arthroscopic Chondroplasty
- Arthroscopic Debridement of the Elbow
- Arthroscopy Of the Ankle
- Articular Cartilage Restoration
- Artificial Disk Replacement (ADR)
- Aspiration of the Olecranon Bursa - Fluid In Elbow
- Atraumatic Shoulder Instability
- Avascular Necrosis (Osteonecrosis)
- Bankart Repair
- Basal Joint Surgery
- Bicep Tendon Tear
- Bicep Tenodesis
- Bone Cement Injection
- Bone Growth Stimulation
- Bone Health Clinic
- Broken Collarbone
- Bunions
- Bursitis of the Shoulder (Subacromial Bursitis)
- Calcific Tendinitis of the Shoulder
- Carpal Tunnel Syndrome
- Charcot Joint
- Chiropractic
- Clavicle Fractures
- Colles’ Fractures (Broken Wrist)
- Common Foot Fractures in Athletes
- Community Outreach
- Cubital Tunnel Syndrome
- De Quervain's Tenosynovitis
- Deep Thigh Bruising
- Degenerative Disk Disease
- Diffuse Idiopathic Skeletal Hyperostosis (DISH)
- Discectomy
- Discitis Treatment & Information
- Dislocated Shoulder
- Dupuytren’s Disease
- Elbow
- Elbow Bursitis
- Elbow Injuries & Inner Elbow Pain in Throwing Athletes
- Epidural Injections for Spinal Pain
- Finger Dislocation
- Flexor Tendonitis
- Foot Stress Fractures
- Foot, Ankle & Lower Leg
- Foraminotomy
- Fractured Fingers
- Fractures Of The Shoulder Blade (Scapula)
- Fractures Of The Tibial Spine
- Functional Nerve Transfers of The Hand
- Ganglion Cysts
- General Orthopedics
- Glenoid Labrum Tear
- Golfer's Elbow
- Groin Strains and Pulls
- Growth Plate Injuries Of The Elbow
- Hallux Rigidus Surgery - Cheilectomy
- Hammer Toe
- Hamstring Injuries
- Hand & Finger Replantation
- Hand & Wrist
- Hand Nerve Decompression
- Hand Skin Grafts
- Hand, Wrist, Elbow & Shoulder
- Heat Injury/Heat Prostration
- High Ankle Sprain (Syndesmosis Ligament Injury)
- Hip & Thigh
- Hip Arthroscopy
- Hip Dislocation
- Hip Flexor Strains
- Hip Fractures
- Hip Hemiarthroplasty
- Hip Impingement Labral Tears
- Hip Muscle Strains
- Hip Pointers and Trochanteric Bursitis
- Hyperextension Injury of the Elbow
- Iliopsoas Tenotomy
- Iliotibial Band Syndrome
- Impingement Syndrome of the Shoulder
- Interlaminar Implants
- Interlaminar Lumbar Instrumental Fusion: ILIF
- Interventional Pain Management
- Interventional Spine
- Intraarticular Calcaneal Fracture
- Joint Replacement
- Knee & Leg
- Kyphoplasty (Balloon Vertebroplasty)
- Kyphosis
- Labral Tears Of The Hip (Acetabular Labrum Tears)
- Laminectomy: Decompression Surgery
- Lateral Collateral Ligament (LCL) Injuries
- Lisfranc Injuries
- Little League Shoulder
- LITTLE LEAGUER'S ELBOW (MEDIAL APOPHYSITIS)
- Lumbar Epidural Steroid Injection
- Lumbar Interbody Fusion (IBF)
- MACI
- Mallet, Hammer & Claw Toes
- Medial Collateral Ligament Injuries
- Meniscus Tears
- Metatarsalgia
- Minimally Invasive Spine Surgery
- Morton’s Neuroma
- Muscle Spasms
- Muscle Strains of The Calf
- Nerve Pain
- Neuromas (Foot)
- Neurosurgery
- Olecranon Stress Fractures
- Orthopaedic Total Wellness
- Orthopaedic Trauma
- Orthopedic Physician Or A Podiatrist? Definition of a Podiatrist
- Osteoarthritis of the Hip
- Osteoporosis
- Outpatient Spine Surgery
- Partial Knee Replacement
- Patellar Fracture
- Pelvic Ring Fractures
- Peripheral Nerve Surgery (Hand) Revision
- Pinched Nerve
- Piriformis Syndrome
- Piriformis Syndrome
- Plantar Fasciitis
- Plastic Surgery
- Podiatry
- Primary Care Sports Medicine
- Quadriceps Tendon Tear
- Radial Tunnel Syndrome (Entrapment of the Radial Nerve)
- Revascularization of the Hand
- Reverse Total Shoulder Replacement
- Rheumatoid Arthritis (RA) of the Shoulder
- Rheumatoid Arthritis Of The Hand
- Robotics
- Rotator Cuff Tears
- Runner's Knee
- Sacroiliac Joint Pain
- Sciatica
- Scoliosis
- Senior Strong
- Shin Splints
- Shoulder
- Shoulder Arthritis
- Shoulder Arthroscopy
- Shoulder Injury: Pain In The Overhead Athlete
- Shoulder Replacement
- Shoulder Separations
- Shoulder Socket Fracture (Glenoid Fracture)
- SLAP Tears & Repairs
- Spinal Fusion
- Spine
- Spondylolisthesis and Spondylolysis
- Sports Foot Injuries
- Sports Hernias (Athletic Pubalgia)
- Sports Medicine
- Sports Wrist and Hand Injuries
- Sprained Ankle
- Sprained Wrist Symptoms and Treatment
- Subacromial Decompression
- Sudden (Acute) Finger, Hand & Wrist Injuries
- Targeted Muscle Reinnervation (TMR)
- Tendon Transfers of The Hand
- Tennis Elbow Treatment
- Thigh Fractures
- Thigh Muscle Strains
- Thumb Ulnar Collateral Ligament Injuries
- Total Ankle Replacement
- Total Hip Arthroplasty
- Total Hip Replacement - Anterior Approach
- Total Knee Replacement Surgery
- Trapezius Strain (Muscle Strain of The Upper Back)
- Traumatic Shoulder Instability
- Tricep Pain & Tendonitis
- Trigger Finger
- Turf Toe
- UCL (Ulnar Collateral Ligament) Injuries
- Ulnar Neuritis
- Valgus Extension Overload
- Vertebroplasty
- WALANT (Wide Awake Local Anesthesia No Tourniquet)
- Whiplash and Whiplash Associated Disorder (WAD)
- Wound Care
- Wrist Arthroscopy
- Wrist Fractures
- Wrist Tendonitis
Services
- Physical Medicine & Rehabilitation
- Physical Therapy
- Primary Care Sports Medicine
- PROMs (Patient-Reported Outcome Measures)
- Same-Day Orthopaedic Appointments Now Available
- Sports Medicine
- Sports-Related Concussion Treatment
- Telehealth Page
- Telemedicine
- Workers' Compensation
- Workers' Compensation Dispensary
- X-Ray
