Scoliosis
Scoliosis is a condition found in children that causes the spine to curve in a “C” or “S” shape. When a child is young, before they hit puberty, the scoliosis is often unnoticeable. But as they grow and go through puberty, the spinal deformities become visible and get worse. There are both surgical and nonsurgical treatments available to help either prevent the spine deformity from getting worse and to completely realign the spine.
Anatomy
The spine consists of 33 individual bones known as vertebrae that interlock. The vertebrae are categorized into five regions:
- Cervical
- Thoracic
- Lumbar
- Sacrum
- Coccyx
About scoliosis
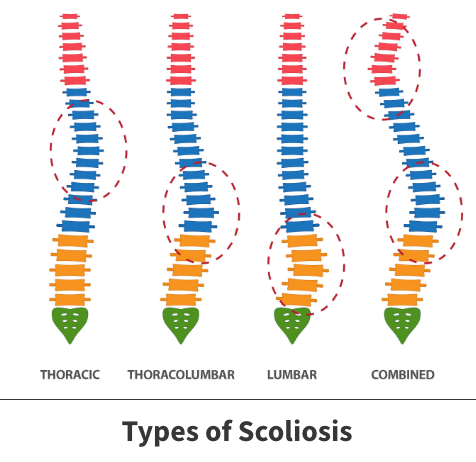
Scoliosis is a condition that causes the bones of the spine to twist or rotate resulting in a deformed spine, shaped more like the letter “C” or “S” rather than a straight line. This deformity most commonly occurs in the upper and middle back (thoracic spine), but it can also affect the lower part of the back.
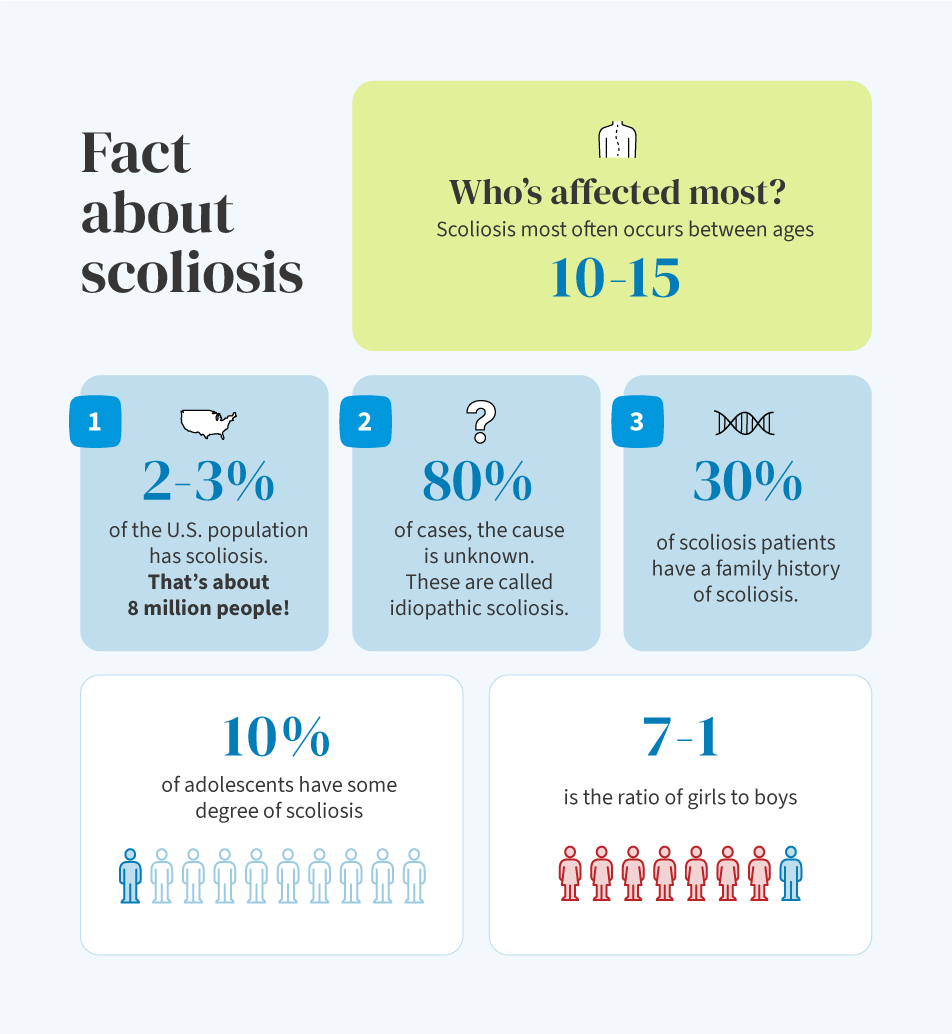
Scoliosis develops in toddlers and young children but symptoms usually do not start appearing until puberty, when the child starts to grow. Both girls and boys and develop scoliosis, but girls are more likely to develop larger curves than boys and are more likely to get the condition.
The curves themselves vary in size. Mild curves are more common than larger ones. If a child is still growing, a scoliosis curve can worsen quickly during a growth spurt if not treated.
Symptoms
Small spinal curves are often unnoticeable until a child hits a growth spurt during puberty.
When symptoms start to show, they include:
- Prominence of ribs on one side
- Tilted, uneven shoulders, with one shoulder blade sticking out more than the other
- One hip higher than the other
- Uneven waistline

Diagnosis
Your Florida Orthopaedic Institute physician will first test for scoliosis by performing the Adam’s forward bend test. During this test, your child will bend forward with their feet together and knees straight. Your physician will observe your child’s back, looking for a difference in the shape of the ribs on each side. This position makes spinal deformities more noticeable and easier to detect.
Additionally, your physician will look at your child standing upright and check if the hips and shoulders are level and if the position of the head is centered over the hips. To rule out other causes of spinal deformity, your physician may also check for abnormal neurological findings, limb-length differences, and other physical issues.
X-rays may also be taken to provide a clear image of your child’s spine. Generally, curves greater than 25° are considered severe enough to need treatment.
Treatment
Your Florida Orthopaedic Institute physician will consider several things when determining the best treatment plan for your child. These things include:
- The severity of the curve
- The location of the curve
- Your child’s age
- The number of remaining growing years
There are both nonsurgical and surgical treatment options available for scoliosis. Surgical treatments are only recommended if the spinal curve is greater than 45°-50° or if nonsurgical treatments are unsuccessful.
Nonsurgical treatments
There are several nonsurgical treatment options available, including:
- Observation – If your child’s spinal curve is less than 25°, or if he or she is almost full-grown, your physician may recommend simply monitoring the curve to make sure it does not get worse. Your physician will recheck your child every 6 to 12 months and schedule X-rays regularly until your child is fully grown.
- Bracing – If the spinal curve is between 25° and 45° and your child is still growing, your physician may recommend bracing. Although bracing will not straighten an existing curve, it often prevents it from getting worse to the point of requiring surgery. There are several different types of braces for scoliosis and are recommended depending on the severity and location of the curve. Most of these braces are underarm braces that are custom made to fit your child comfortable. Braces can be hidden under clothing and can be taken off for sports activities.
Surgical treatments
Surgery may be recommended if bracing did not work or if your child’s spinal curve is greater than 45°-50°. Spinal fusion is the primary surgical procedure used to straighten the spine. During this procedure, the spinal bones that make up the spinal curve deformity are realigned. Small pieces of bone (bone graft) are placed into the spaces between the vertebrae and fused together with the realigned section of the spine. Metal rods are usually used to hold the bones in place until the fusion happens, attached to the bone using hooks, screws, and wires. Only the deformed section of the spine is fused together, everything else is left alone.
This procedure will stop growth in the part of your child’s spine that is affected by scoliosis.
By the second day after surgery, most patients are able to walk without a brace and are usually discharged from the hospital less than a week following surgery. Most children can return to school and resume daily activities within a month. Sports activities can be resumed 6 to 9 months.
Videos
Related specialties
- Anterior Cervical Corpectomy & Discectomy
- Artificial Disc Replacement (ADR)
- Bone Cement Injection
- Degenerative Disc Disease
- Diffuse Idiopathic Skeletal Hyperostosis (DISH)
- Discectomy
- Discitis Treatment & Information
- Epidural Injections for Spinal Pain
- Foraminotomy
- Interlaminar Implants
- Interlaminar Lumbar Instrumental Fusion: ILIF
- Kyphoplasty (Balloon Vertebroplasty)
- Kyphosis
- Laminectomy: Decompression Surgery
- Lumbar Epidural Steroid Injection
- Lumbar Interbody Fusion (IBF)
- Minimally Invasive Spine Surgery
- Outpatient Spine Surgery
- Pinched Nerve
- Piriformis Syndrome
- Sacroiliac Joint Pain
- Sciatica
- Spinal Fusion
- Spondylolisthesis & Spondylolysis
- Vertebroplasty
- Whiplash & Whiplash Associated Disorder (WAD)
