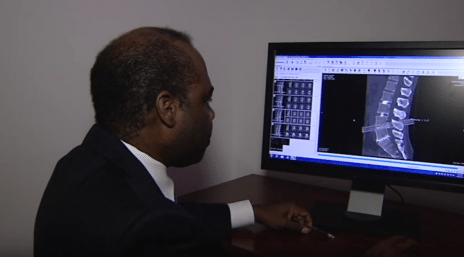
Leading care from interventional pain specialists
Treatments for chronic pain
Florida Orthopaedic Institute pain management specialists understand that living with chronic pain can turn simple tasks into daily challenges. Interventional pain management (also called interventional spine) treats pain with various techniques such as facet joint injections, nerve blocks, radiofrequency ablation, and implant, and epidural injections. Our interventional pain specialists are patient-focused experts at developing non-surgical, individualized plans that address persistent pain.

Learn more about
Interventional pain specialists









Common pain management conditions
FOI interventional pain specialists are experts at addressing chronic pain resulting from the following conditions:
- Annular Tear
- Bulging Disc
- Cervicogenic Headache
- Cervical Radiculopathy (Pinched Nerve in the Neck)
- Complex Regional Pain Syndrome (CRPS)
- Degenerative Disc Disease
- Discitis
- Disc Extrusion
- Disc Protrusion
- Facet Joint Arthritis
- Failed Back Surgery Syndrome
- Herniated Discs
- Neck & Spine Pain
- Occipital Neuralgia
- Sacroiliitis (Sacroiliac Joint Pain)
- Sciatica
- Spinal Stenosis
- Spondylolisthesis & Spondylolysis
- Whiplash Injuries (Neck Strains) & Whiplash-Associated Disorders
“I was experiencing back pain for over three months. Dr. Epting suggested doing an epidural injection. The day following the epidural injection, I felt the best I had in months and back to my usual self. It's hard to find good providers with good office staff, and Florida Orthopaedic seems to be figuring out how to keep the excellent staff.” Patient | Interventional Spine
A multidisciplinary approach
Interventional pain management is a multidisciplinary approach. A team of health care professionals works together to provide a full range of treatments and services for patients suffering from chronic and acute pain. Sometimes the techniques may be used in conjunction with mental and emotional therapy and prescription medications.
Working with your primary care physician (or another physician who has referred you), your medical team may include the following health care professionals: physical & occupational therapists, psychologists & psychiatrists, anesthesiologists, and physiatrists.
The most important member of the team is you. That’s because interventional pain management relies on the full cooperation of patients throughout the treatment process for a successful outcome.
Treatments from interventional pain specialists
Our leading interventional pain specialists use the following exceptional, minimally invasive techniques to relieve chronic back and neck pain:
A cervical epidural injection is an injection of medicines into the neck, into the area around your spinal cord. This outpatient procedure can help with pain, numbness, or tingling in your neck, shoulder, or arms. Cervical epidural injections may contain steroids to reduce swelling and pain, as well as an anesthetic to numb the nerves. Sometimes, only a steroid is used.
Different people have different results from cervical epidural injections. Some get relief within a day. Others may take up to five days, or not see any results at all. Relief from pain can last for several days or up to a few months.
Cervical radiofrequency ablation (RFA) is an outpatient procedure for treating pain in the upper back, neck and shoulder. It is also called rhizotomy or cervical facet thermal coagulation.
Facet joints connect the bones of the spine (vertebrae) There are seven vertebrae in the neck area, called the cervical region. About the size of a thumbnail, facet joints are found on both sides of the spine. They help guide your spine during movement. When a cervical facet joint is injured, the medial branch nerve communicates pain. The pain can range from a feeling of muscle tension to severe pain. Sometimes the injury is from the cartilage inside the joint, but the ligaments surrounding the joint can also be injured.
How do you know if you have cervical facet pain? If you have pain in one or more areas from your neck down to your 7th cervical vertebrae and it lasts longer than two months you may have cervical facet pain. Since common tests such as an X-ray or MRI may not show if a facet joint is causing the pain, your physician can diagnose it by blocking the pain signal. A local numbing agent (anesthetic) is used on the medial nerve branch.
Cervical RFA uses radiofrequency energy to disrupt nerve function. This keeps the cervical medial nerve branch from transmitting pain signals for the injured facet joint.
Epidural injections can be very beneficial in providing relief for patients during an episode of severe back pain, reducing inflammation associated with common conditions such as spinal stenosis, disk herniation or degenerative disk disease. An epidural steroid injection for pain involves injecting a steroid around the dura, the sac near the nerve roots that contains cerebrospinal fluid, to remove inflammatory proteins that may cause pain. Epidural steroid injections are successful in relieving lower back pain for approximately 50% of patients. The effects of the injection may be temporary (one week to one year).
A lumbar facet injection delivers a local numbing medicine (anesthetic) and anti-inflammatory medicine (corticosteroid) into one or more of your lumbar facet joints. The injection is used to both diagnose or treat your pain. The anesthetic lessens the pain temporarily, while the corticosteroid treats the inflammation of the facet joint. If the injection lessens your pain and helps you move better, the doctor can determine which facet joint may be causing the pain.
Medial branch nerves carry the pain messages from your facet joints. Radiofrequency medial branch neurotomy is used to relieve pain by using radio waves to neutralize nerves in your neck or back, preventing them from sending pain messages to your brain. Your doctor will do a medial branch block first to find out if certain nerves are a source of your pain. This helps determine if a neurotomy will help you. After a successful neurotomy, most people have immediate pain relief that can last for 9 to 12 months or longer.
Nerve block injections are used to treat pain associated with a nerve. Nerve pain in a joint may be caused by arthritis, injury, and degeneration. An injection temporarily prevents the pain and can identify whether the sensory nerves are the true source of your pain. The effects of a nerve block are typically temporary.
Your physician may recommend alternating over-the-counter medication options, such as Tylenol (acetaminophen) and aspirin, Motrin, and Advil (non-steroidal anti-inflammatory drugs-NSAIDs) as an equally effective opioid alternative for controlling pain. Non-drug therapies used alone or in combination with drugs, such as physical therapy, acupuncture, surgery, injections, and nerve blocks can also provide pain relief.
Bones surrounding the sacroiliac joints are uneven. These jagged edges help keep surrounding bones and other parts together. Also, the spaces near these bones are covered by nerve endings, which send pain signals to the brain. When joints, neighboring bones, muscles, or tissues are injured or diseased, pain and other symptoms can develop. This condition is known as sacroiliac joint dysfunction or sacroiliitis. Nonsurgical sacroiliac joint pain treatments include radiofrequency ablation, sacroiliac joint steroid injections, heat and cold applications, low-impact exercise, and over-the-counter medications.
Spinal cord stimulation is used to treat consistently acute pain that cannot be relieved through more conventional treatments. A spinal cord stimulation is a two-step process:
- Electrical leads are implanted in the spinal cord or affected nerve(s).
- A small generator is then inserted in your back just under the skin.
This directs a power-driven current to the spinal cord. You feel a sensation of tingling that replaces your pain.
Trigger point injections are used to care for painful muscle knots. Trigger points can aggravate adjacent nerves which causes the pain to spread and even sometimes circulate to other areas. This procedure is also a minimally invasive one and is administered by injecting a dose of corticosteroid directly into the affective area. A trigger point injection is typically successful at relieving the pain.