Exceptional care from knee reconstruction specialists
Treatments for leg & knee pain
The muscles, tendons and bones inside our knees and legs form an intricate system that allows us to run, squat, jump, and turn. Given their complexity, treatment for leg and knee pain requires the highest level of expertise.






Learn more about
Knee & leg specialists at FOI






























Common knee & leg conditions
The knee and leg are supported by a complex system of moving parts, including bones, cartilage, muscles, tendons, and ligaments. Each of these parts is subject to injury or disease, such as:
- Anterior Cruciate Ligament (ACL) Injuries
- Arthritis
- Deep Thigh Bruising
- Fractures of the Tibial Spine
- Iliotibial Band Syndrome (ITBS)
- Joint Replacement
- Lateral Collateral Ligament (LCL) Injuries
- Medial Collateral Ligament (MCL) Injuries
- Meniscus Tears (Cartilage)
- Muscle Spasms
- Muscle Strains of the Calf (Gastrocnemius & Soleus Strains)
- Osteoarthritis
- Patellar Fractures
- Quadriceps Tendon Tears
- Runner’s Knee
- Shin Splints

Learn more about the questions you should ask when meeting with your knee pain specialist.
“It’ll be a year in June since I got my knee replaced. It’s the fourth best thing I ever did. The first best was, of course, marrying my wife. The second and third were my two kids being born. And the fourth was getting my knee done. It's been great.” Bob Aijala | Partial Knee Replacement
Treatments from knee pain specialists
Our internationally renowned physicians offer the following results-driven leg and knee pain treatments, performing surgery only when necessary:
Arthroscopic chondroplasty is an outpatient procedure that is used to repair a small area of damaged cartilage in the knee. During the procedure, damaged tissue is removed, allowing healthy cartilage to grow in its place. Arthroscopic chondroplasty is performed through small incisions on the sides of the knee with the aid of a small video camera called an arthroscope.
The smooth, white tissue that covers the ends of bones where they come together to form joints is your articular cartilage. Healthy cartilage allows the bones to glide over each other with very little friction and makes it easier to move. Injury or normal wear and tear can damage articular cartilage. Surgical techniques have been developed to stimulate the growth of new cartilage because cartilage does not heal itself well. When articular cartilage is restored, it allows better function, relieves pain, and delays or prevents arthritis onset. There are many surgical techniques to repair damaged cartilage, some of which are still evolving.
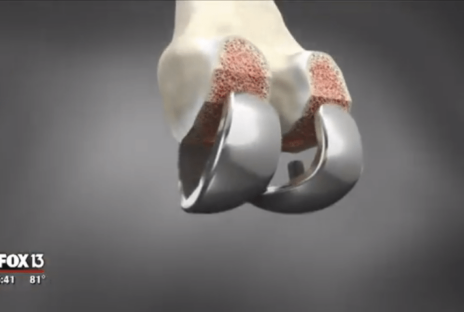
ConforMIS® knee replacement implants are individualized by patient, with no two alike. Each implant is sized and shaped to fit each patient’s unique anatomy, offering advantages over other knee implants. The ConforMIS knee replacement systems offer unique advantages over other implants, such as reduced residual pain after surgery, a more natural feeling knee and a design that preserves the optimal amount of bone. Pre-navigated instrumentation and surgical planning images verify accuracy throughout the surgery. The cost is covered by many major insurance companies similar to a standard total knee replacement.
MACI technology uses the patient’s own cells to treat cartilage defects in the knee. MACI is done through smaller incisions with significant improvements in operating time and an easier path to recovery. While this technology is new in the United States, it has an almost 10-year track record in Europe with excellent results. MACI helps many patients avoid early partial and total joint replacements by restoring the cartilage surface of their knee before the problem progresses to a much worse situation.
In 2016, Florida Orthopaedic Institute performed an innovative and sophisticated total knee replacement surgery using the Mako robotic-arm assisted surgery system. The Mako system is a surgeon-controlled robotic arm technology that enables accurate alignment and placement of implants. Before the surgery, the Mako robotic-arm assisted surgery system creates a 3-D model of your knee to pre-plan the procedure. Your surgeon guides the robotic arm, using the pre-plan guidelines, and removes only the diseased bone. A tremendous advantage of this procedure is that it preserves your healthy bone and soft tissue as well as assisting the surgeon in positioning your implant.
The NAVIO® surgery system allows Florida Orthopaedic surgeons to perform precise and accurate partial knee replacements. As the first and only location in Florida with the NAVIO® robotic assisted surgical system (and one of only 79 locations worldwide), Florida Orthopaedic surgeons can visualize their patient’s X-rays. By making partial knee replacements a more accessible option through improved precision, patients receive a surgical procedure that is generally associated with smaller incisions, less scarring, and quicker recovery when compared to the total knee replacement alternative.
Knee osteoarthritis occurs when the cartilage protecting the bones of the knee slowly wears away. Osteoarthritis can appear throughout the knee joint or just in a single area of the knee. If advanced osteoarthritis is limited to a single compartment of the knee, it can be treated with a unicompartmental knee replacement. During a partial knee replacement, damaged bone and cartilage are resurfaced with metal and plastic components. The procedure preserves healthy cartilage, bone, and all of the ligaments. This procedure is an alternative to total knee replacement for patients whose disease is limited to just one area of the knee.
The ROSA® Knee is a robotic surgical assistant for total knee replacement. ROSA® Knee provides your surgeon with data about your knee which is then used to create a plan for your surgery based on your unique anatomy. The ROSA® Knee does not operate on its own, as the surgeon is in the operating room the entire time making decisions throughout the surgery. ROSA® Knee uses a camera and optical trackers to know where your leg is in space. If your leg moves, the robot can tell and adjust accordingly.
When the knee joint is affected by osteoarthritis or rheumatoid arthritis and non-surgical methods have not decreased the knee pain, total knee replacement surgery (total knee arthroplasty) is a highly successful option. This procedure replaces the infected and painful knee joint with an artificial joint made of state-of-the-art materials.
If you’re considering knee replacement, VERILAST® knee technology addresses one of the most commonly cited concerns associated with knee replacement implants – implant wear. For the plastic inserts, XLPE (a special high density polyethylene) reduces the amount of wear against the metal component. The thigh bone portion of the VERILAST® implant is made from OXINIUM Oxidized Zirconium – a process that transforms the implant’s surface into a hard, ceramic metal. It’s more than twice as hard and twice as scratch-resistant as a cobalt chrome implant.