Articular cartilage restoration
You likely know the critical role physical features like muscles and bones play in helping you stand, walk, and carry out almost every other vital function.
You might not know that other internal components, including soft tissues, carry out a crucial part in ensuring your muscles and bones remain strong and healthy. One such component is known as articular cartilage.
When this material becomes damaged, you can experience many uncomfortable and possibly debilitating symptoms. They can be eased through procedures called articular cartilage restoration.
Anatomy
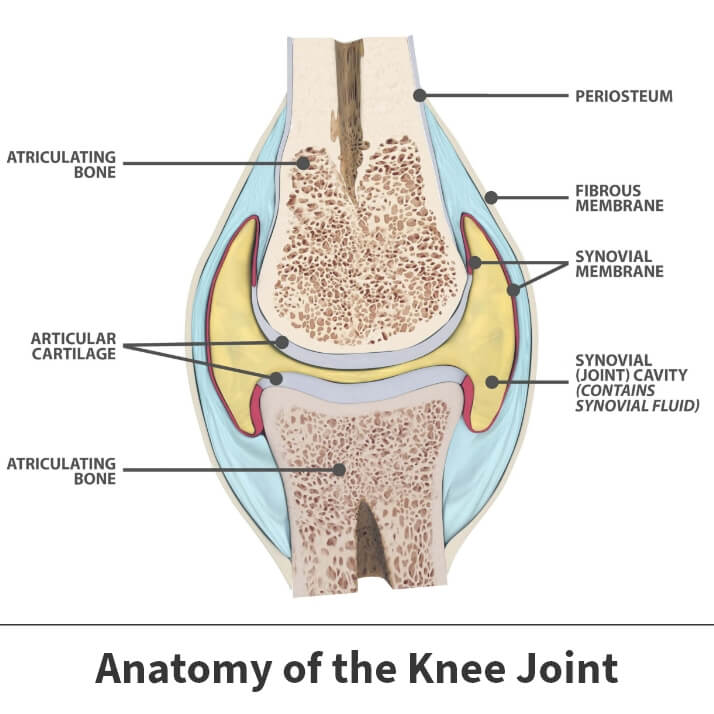
Articular cartilage is a relatively soft material cushioning bones where they contact the joints holding them together. When cartilage is healthy and abundant, your bones can move with greater ease and encounter less friction.
About
Cartilage damage often results from some type of acute, traumatic injury that impacts bones and joints. Natural deterioration can also take place over time.
Causes
Cartilage damage usually results from one of three common causes: a major injury, gradual wear and tear, and a lack of movement.
Major injury
A significant percentage of cartilage damage results from some type of dramatic and direct injury. This frequently occurs in sporting events involving physical contact between competitors, including:
- Rugby
- Football
- Wrestling
- Basketball
Injuries can also happen following traumatic occurrences like severe falls and auto accidents.
Age
As you age, cartilage gradually breaks down. Your bones are used every day executing typical, routine movements. Decades of walking, climbing stairs, bending, and lifting forces force your knees and ankles to exert effort. This can weaken cartilage over time.
Inactivity
Remaining inactive does not benefit your joints. Prolonged periods of inactivity can result in cartilage damage or speed up its deterioration.

Symptoms
Damaged articular cartilage often produces a noticeable amount of pain. Such discomfort can worsen when you engage in certain activities.
Besides pain in the affected joint, you might also encounter inflammation. Inflamed or irritated joints might have redness and swelling. Surrounding tissues might also feel warm and tender to the touch.
You may experience significant stiffness. This can cause your knees, shoulders, wrists, ankles, and elbows to grow increasingly difficult to move.
Complications
Cartilage damage is a progressive issue and only worsens with time. Failing to receive a proper diagnosis and treatment can lead to more serious concerns like life-limiting pain and even permanent joint damage.
Articular cartilage restoration
Once cartilage is damaged, it is slow to heal. Physicians have created many methods to help cartilage regenerate. These processes are known as articular cartilage restoration.
Treatment
Articular cartilage restoration is a broad term used to describe any number of surgical procedures. Some undertakings are more invasive than others. Your doctor will determine which one most suits your needs after considering several issues, such as your age, weight, level of physical activity, overall health, the region where the cartilage damage is located, and the severity of the problem.
Surgical Procedures
- Drilling – Surgeons drill holes into the bones beneath the affected cartilage – the subchondral region. This opening of the bone, which is typically performed using a minimally invasive surgical tool called an arthroscope, stimulates the healing process by creating a new and increased blood supply to the damaged area.
- Microfracture – Similar to drilling, surgeons create holes in the joint in the subchondral area. This process is done using an instrument called an awl. These openings form a pathway for fresh blood supplies to reach damaged tissue and start healing.
- Abrasion arthroplasty – During this procedure, surgeons use tools (burrs) to extract injured cartilage and create openings in subchondral bones.
- Osteochondral autograft transplantation – Surgeons remove cartilage from a healthy joint and transplant it into the damaged joint. This procedure is scientifically referred to as grafting.
- Autologous chondrocyte implantation – Often abbreviated as ACI, cells are formed to create new cartilage and then placed into the damaged joints. This procedure is a multi-step process.
- The first phase involves the removal of a small amount of healthy cartilage. Cartilage cells (chondrocytes) are then extracted and multiplied inside a laboratory setting for several weeks.
- Once enough chondrocytes are created, they are placed into the receiving joint in an open surgical procedure.
- Osteochondral allograft transplantation – This procedure is similar to autograft transplantation. It uses cartilage samples taken from cadavers instead of from your own body.
Prognosis
Regardless of the restoration procedure performed, there will be a recovery period. Movement-constructing devices will cover the joint and surrounding tissues in question while the healing process progresses. If performed on your knee or ankle, you might additionally need crutches or walking boots for several weeks.
Your doctor will likely prescribe physical therapy. These are specially designed exercises geared towards helping the healing joint recapture lost motion and regain its strength.
Specific recovery times are difficult to determine. Healing often occurs faster following arthroscopic based procedures. Everyone heals at their own pace. Underlying issues like age, physical condition, and general health will likely factor into specific time frames.
Videos
Related specialties
- ACL Injuries
- Arthroscopic Chondroplasty
- Deep Thigh Bruising
- Fractures of the Tibial Spine
- Iliotibial Band Syndrome
- Lateral Collateral Ligament (LCL) Injuries
- MACI
- Medial Collateral Ligament Injuries
- Meniscus Tears
- Muscle Spasms
- Muscle Strains of the Calf
- Partial Knee Replacement
- Patellar Fracture
- Quadriceps Tendon Tear
- Runner's Knee
- Senior Strong
- Shin Splints
- Total Knee Replacement Surgery
