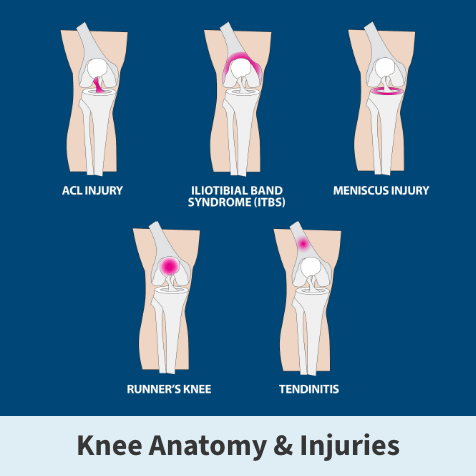
ACL tears
An anterior cruciate ligament (ACL) sprain or tear is one of the most common knee injuries. High-demand sports like soccer, football, and basketball have a higher incidence of ACL injuries.
An injury to the anterior cruciate ligament may need surgery to regain full function of the knee, depending on the severity of your injury, activity level, general health, and other factors.
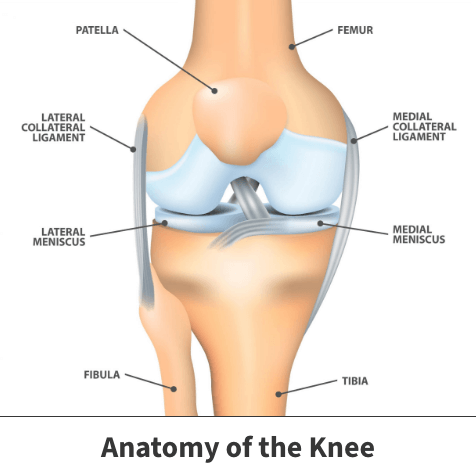
Anatomy
The knee is a hinged joint with four main parts: bones, cartilage, ligaments, and tendons. The thighbone (femur), shinbone (tibia), and kneecap (patella) meet to form the knee joint. The kneecap helps protect the front of the joint.
About
Ligaments connect bones to one another and keep the knee stable. The knee has four primary ligaments of two types:
Collateral Ligaments – on the sides of the knee, controlling the sideways motion of the knee and bracing it against unusual movement.
- Medial collateral ligament (MCL) on the inside
- Lateral collateral ligament (LCL) on the outside
Cruciate Ligaments – located inside your knee joint, controlling the back-and-forth motion of the knee.
- Running diagonally in the middle of the knee, the anterior cruciate ligament (ACL) prevents the shinbone (tibia) from sliding out in front of the thighbone (femur) and provides rotational stability.
- The posterior cruciate ligament (PCL) mirrors the ACL but is attached to the back of the knee, crossing the ACL in an X.
A layer of articular cartilage covers the weight-bearing surface of the knee. The medial meniscus and lateral meniscus are between the cartilage surfaces of the thighbone and shinbone on either side of the joint. They act as shock absorbers and work with the cartilage to reduce stress between the shinbone and the thighbone.
ACL injuries
The ACL is a cruciate ligament located inside the knee and helps it bend and stretch. The ACL provides stability by preventing the shinbone and thighbone from colliding. When the ligament is overextended or exposed to extra force, it can become injured.
Your anterior cruciate ligament can be injured in several ways:
- Rapidly changing direction
- Deceleration coupled with cutting, pivoting, or sidestepping moves
- Suddenly stopping
- Slowing down while running
- Awkward or incorrect landings from a jump
- Out-of-control play
- Direct contact or collision (like a football tackle)
Most ACL injuries occur through non-contact; a smaller percentage are from direct contact with another player or object.
Risk factors
Female athletes tend to have a higher incidence of ACL injuries than males in certain sports. This may be due to differences in physical conditioning, muscular strength, neuromuscular control, differences in pelvis and lower leg alignment, increased looseness in ligaments, and the effects of estrogen.
Half of ACL injuries happen when there is damage to other structures in the knee, such as the meniscus, articular cartilage, or other ligaments. There can also be bruising of the bone beneath the cartilage surface. Magnetic resonance imaging (MRI) scans can help see these additional injuries. Football players and skiers commonly injure the ACL, the MCL, and the medial meniscus, nicknamed the “unhappy triad.”
Get more information about ACL tears and other common pickleball knee injuries.
ACL grades
ACL damage is medically classified as a sprain. Based on their seriousness, these injuries are graded on a severity scale into three categories.
- Grade 1 sprains – The ligament is mildly damaged. It has been slightly stretched but can still help keep the knee joint stable. The ligament was overextended but not damaged.
- Grade 2 sprains – The ligament is stretched to the point where it becomes loose. It is also referred to as a partial tear of the ligament. Partial tears are rare – most ACL injuries are complete or near-complete tears.
- Grade 3 sprains – Grade three events are the most significant and involve complete ligament tears. The ligament is split into two pieces, and the knee joint is unstable. This is commonly called a complete ligament tear. Grade 3 sprains greatly limit mobility and usually cause major knee instability

Symptoms
Symptoms tend to vary depending on grade severity. When the anterior cruciate ligament is injured, typical symptoms include:
- A “popping” noise
- The knee gives out from under you
- Loss of range of motion
- Tenderness along the joint line
- Discomfort while walking
- Pain with swelling – Within 24 hours after the injury, the knee swells. Sometimes, the swelling and pain resolve on their own. You risk causing further damage to the cushioning cartilage (meniscus) of your knee if you return to sports, as your knee may be unstable
If not identified and treated quickly, ACL tears can worsen. Additionally, these injuries can negatively impact other knee components leaving you at greater risk of developing other painful and potentially life-impacting issues.
ACL diagnosis
Your Florida Orthopaedic Institute physician will check all the structures of your injured knee and compare them to your non-injured knee during a physical examination.
Most ligament injuries can be diagnosed with a thorough physical examination of the knee. They will also ask you about your symptoms and medical history.
Other tests that help your doctor confirm a diagnosis include X-rays and MRI scans. Although X-rays don’t show injuries to your anterior cruciate ligament, they can show whether the injury is associated with broken bones.
MRI scans (magnetic resonance imaging) create a better image of your soft tissues like anterior cruciate ligaments.
Your physician may also perform a Lachman Test, which tests the movement of the knee. The test helps identify the anterior cruciate ligament’s integrity and gauges instability in various directions.
Treatment
The specific treatment chosen by a Florida Orthopaedic Institute physician will depend on the patient’s age, health, sprain severity, and activity level. For example, younger competitive athletes will likely need surgery in all but the mildest instances if they desire a quicker return to their sport. Often older, less active persons can avoid surgery.
Partial tears do not always need surgery. Recovery most often comes after treatment, a course of physical therapy, and several thorough follow-ups with orthopedic doctors to prevent potential issues like lingering pain and instability.
Complete ruptures usually need surgery. It is also important to note that ACL tears can lead to damage elsewhere in the knee. Close monitoring of the knee should occur following these events.
Certain types of ACL injuries stand the best chance of healing without surgery, including:
- Complete tears with no symptoms in individuals competing in low contact sports
- Partial tears with no signs of instability
- Persons employed in sedentary jobs or those requiring little physical labor
- Those occurring in growing children
- If the knee’s stability seems intact, it may be suitable for nonsurgical treatments
Nonsurgical treatments
Torn ACLs do not heal without surgery, but nonsurgical treatment may be effective for older patients or have very low activity levels. Nonsurgical healing varies from patient to patient and depends on their activity level, the degree of injury, and knee instability.
A positive outcome for partially torn ACLs without surgery is possible, with the recovery and rehabilitation period typically lasting at least three months. Some patients with partial ACL tears may still have instability symptoms. Comprehensive clinical follow-up and physical therapy help identify patients that have unstable knees from partial ACL tears.
Without surgical intervention, complete ACL ruptures have a much less favorable outcome. After a complete ACL tear, some patients have instability during walking or other normal activities. Athletes are usually unable to participate in sports that involve cutting or pivoting movements, but a few can participate without any symptoms of instability. It all depends on the severity of the original knee injury and the patient’s physical demands.
Secondary damage to the meniscus, articular cartilage, or other ligaments can occur in patients with repeated knee instability. With chronic instability, most patients have meniscus damage ten or more years after the initial injury.
With progressive physical therapy and rehabilitation, most knees can be restored to a condition close to their pre-injury state. Patients have to learn how to prevent instability and may need to use a hinged knee brace.
These types of isolated ACL tears have better nonsurgical success:
- Partial tears with no instability symptoms
- Complete tears with no symptoms of knee instability during low-demand sports, and patients who are willing to give up high-demand sports
- Those with light manual work or sedentary lifestyles
If the overall stability of the knee is intact, your Florida Orthopaedic Institute physician may recommend these nonsurgical options:
- Bracing – Protects your knee from instability. You may also be given crutches to keep you from putting weight on your leg to protect your knee further.
- Crutches – Crutches prevent the recovering patient from placing weight on the healing knee.
- Physical therapy – A rehabilitation program can be started as soon as the swelling goes down. Specific exercises can restore function to the knee and strengthen the leg muscles supporting it.
Surgical treatments
Florida Orthopaedic Institute doctors often recommend surgery when patients have ACL tears in combination with other knee injuries.
ACL repair can often be performed through a procedure known as arthroscopy. Surgeons often favor this approach because it is less invasive, can be done as an outpatient procedure, requires less time in hospital, reduces post-surgical pain, and faster recovery time. Additionally, arthroscopy can also be used to correct other knee damage.
Learn More About Outpatient Surgery
The patient may need surgery to fix the damaged ligament and recapture knee stability in more serious instances. Unfortunately, most damaged ACL tears cannot simply be put back together.
Torn ligaments must be replaced with grafts. These are structures built out of tissues located in other body areas or from deceased individuals. Once grafts are attached, they are fastened to the bone.
ACL arthroscopic procedure
Your physician may recommend knee arthroscopy if your condition does not respond to nonsurgical treatments, and you have pain. Surgery to rebuild an anterior cruciate ligament can be done with an arthroscope using small incisions, and the procedure is less invasive.
Knee arthroscopy can also relieve painful symptoms of many problems that damage the joint’s cartilage surfaces and other soft tissues. Other arthroscopic procedures for the knee include:
- Torn anterior cruciate ligament reconstruction
- Removal of inflamed synovial tissue
- Removal of loose fragments of bone or cartilage
- Removal or repair of a torn meniscus
- Treatment of knee infection (sepsis)
- Treatment of kneecap (patella) problems
- Trimming of damaged articular cartilage
Rebuilding the ligament
To surgically repair the ACL and restore knee stability, the ligament must be reconstructed as most ACL tears cannot be stitched (sutured) back together. ACL repairs done this way generally fail over time. The torn ligament is replaced with a tissue graft to act as a framework for a new ligament to grow on.
Grafts are obtained from several sources. If they come from the patient, they are called autografts. Grafts are often taken from the patellar tendon, which runs between the kneecap and the shinbone (patellar tendon autograft). Hamstring tendons at the back of the thigh (hamstring tendon autograft) and quadriceps tendons (which runs from the kneecap into the thigh and is called a quadriceps tendon autograft) are also common sources of grafts. Cadaver grafts (allografts) are also used and taken from the patellar tendon, Achilles’ tendon, semitendinosus, gracilis, or posterior tibialis tendon.
Your Florida Orthopaedic Institute surgeon will review the advantages and disadvantages of various graft sources to help determine which is best for you.
Because regrowth takes time, it can take six months or more before an athlete can return to sports after surgery.
Rehabilitation after ACL treatments
Rehabilitation plays a vital role in getting you back to your daily activities, whether your treatment involves surgery or not. Physical therapy programs help regain knee strength and motion.
Following surgery, physical therapy focuses initially on returning motion to the joint and surrounding muscles, followed by a strengthening program to help protect the new ligament. Strengthening exercises gradually increase the stress across the ligament. For athletes, the final rehabilitation phase is designed to create a functional return to their sport.
Active adult patients whose jobs involve pivoting, turning, or heavy manual labor should consider surgical treatment, as well as those who actively play sports. Activity, not age, typically determines surgical consideration.
Your surgeon may delay ACL surgery in young children or adolescents until they are closer to skeletal maturity. They may also change the ACL surgery technique to decrease the risk of growth plate injury and bone growth problems.
Surgical treatment may be necessary for combined injuries as it generally produces better outcomes. Almost half of meniscus tears are repairable and can heal better if the repair is done along with the ACL reconstruction.
Pickleball for seniors: 10 tips for pain-free play
Related specialties
- Arthroscopic Chondroplasty
- Articular Cartilage Restoration
- Deep Thigh Bruising
- Fractures of the Tibial Spine
- Iliotibial Band Syndrome
- Lateral Collateral Ligament (LCL) Injuries
- MACI
- Medial Collateral Ligament Injuries
- Meniscus Tears
- Muscle Spasms
- Muscle Strains of the Calf
- Partial Knee Replacement
- Patellar Fracture
- Quadriceps Tendon Tear
- Runner's Knee
- Senior Strong
- Shin Splints
- Total Knee Replacement Surgery
