Tibial spine fracture
Fractures of the tibial spine occur in the section of the leg at the top of the shin and directly below the knee. This type of fracture is relatively uncommon and typically occurs from a high-impact injury such as a hard fall or car accident. It is also most common in children ages 8-14 but also happens to adults. Surgery is the primary treatment type for this injury. But if your bone does not shift out of place during the fracture, then nonsurgical treatments such as braces can work better than surgery. Your specific treatment plan is entirely dependent on the severity of your injury and your physician’s recommendations.
Anatomy
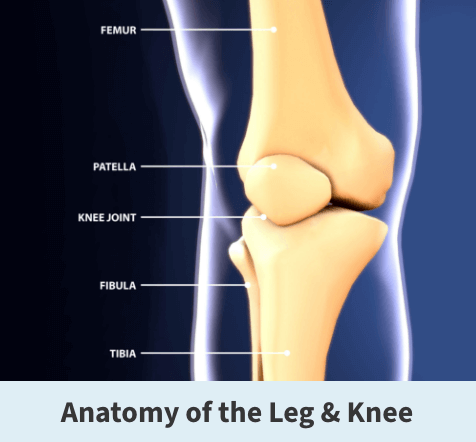
The lower leg is made up of two bones: the tibia and fibula. The tibia is the larger of the two bones. It supports most of your weight and is an essential part of both the knee joint and ankle joint. The tibial spine is a specialized ridge of bone in the tibia where the anterior cruciate ligament (ACL) attaches. This ligament is integral maintaining flexibility and stability in the knee.
About
A tibial spine fracture is a relatively uncommon injury that results in a fracture or break in the shin bone just below the knee which is at the base of the tibial spine. The tibial spine can break straight across, which is known as a transverse fracture. It can also break into many pieces, which is a comminuted fracture. These fractures can also extend into the knee joint and separate the surface of the bone into several parts. These types of fractures are called intra-articular or tibial plateau fractures.
While tibial spine fractures can occur in adults, they are most common in children ages 8-14 because of their skeletal immaturity. Tibial spine fractures are typically caused by the stress from a high-intensity activity, a hard impact to the bone, or from an already compromised or weakened bone. Usually younger people will get a tibial spine fracture from a hard impact injury, such as a fall from a height or a sports-related injury. Older people tend to get a tibial spine fracture from weaker bones or a small injury.
Tibial spine fractures create traction forces along the ACL (anterior cruciate ligament) and cause the tibial spine to be pulled or torn apart. This makes the immature tibial spine weaker than the ACL. The sooner a tibial spine fracture is recognized, the sooner it can be treated, which will minimize any long-term complications.
Symptoms
The most common symptom of a tibial spine fracture is acute pain in the front or center of the knee. But you may also experience swelling, bruising, or weakness in the knee.
Diagnosis
Your Florida Orthopaedic Institute physician will take a look at your symptoms and overall medical health and history to help determine if you have fractured your tibial spine. Your physician will also examine the soft tissue surrounding the knee joint, checking for bruising, swelling, and open wounds. They will also check the nerve and blood supply of your injury.
Your physician may order some tests to help determine if you have a fractured tibial spine and not a different injury. These tests include:
- X-rays – X-rays provide clear images of bone and produce an image of your fractured tibial spine.
- CT scan – This test shows more detail about your fracture, which will help your physician to determine the best way to treat your injury.
- MRI scan – This test produces clear images of the soft tissues, such as tendons and ligaments, in your leg. Although it is not a routine test for tibia fractures, your doctor may order an MRI scan to help determine if there are more injuries to the soft tissues surrounding your knee.

Treatment
Surgical treatments are the primary treatment for tibial spine fractures. Nonsurgical treatments are only recommended if the fracture is not severe, meaning that the bone has not shifted out of position. Both result in a full recovery.
Nonsurgical treatments
If your tibial spine fracture is not severe, then your physician may prescribe casting and bracing with restrictions on motion and weight-bearing. This treatment plan will also need additional, regular X-rays throughout your recovery to monitor whether the bones are healing correctly. Knee motion and weight-bearing activities begin as the injury and method of treatment allow. This type of treatment typically takes about six weeks.
Surgical treatment
There are two main steps to a tibial spine fracture surgical procedure. First, the broken tibial spine bones are realigned. After, depending on the fracture, the bones may need to be held in place with sutures, screws, or a different material. Locking the bone fragments together is known as fixation.
During the surgical procedure for tibial spine fractures, tiny incisions are made on the front side of the shin. An small camera (arthroscope) is inserted into the leg through one of the incisions while surgical instruments are inserted through the remaining incisions. Once everything is set up, the hematoma (a solid swelling of clotted blood within the tissues) is removed using a device known as a motorized suction shaver. The bone fragments are then identified, and all soft tissues in the area are removed, giving your surgeon a better view of the injury. The knee is examined for any other injuries, such as an entrapped meniscus and any other soft tissues, are pulled back so that the fracture can be repaired.
Fixation can be done using either cannulated screws or non-absorbable sutures. Screw fixation works best in cases where the bony fragment is large enough and in patients in whom the growth plate is closed or fused completely. However, in children with open growth plates and when the piece is not large enough to accommodate a screw, a non-absorbable suture may be used.
After the procedure, your physician will prescribe pain medication to help make your recovery easier. Eventually, your physician will determine when it is time for you to begin moving your knee. This depends on how well the soft tissues are recovering and how secure the fracture is after having been fixed. Early motion sometimes starts with passive exercise. A physical therapist will gently move your knee for you, or your knee may be placed in a continuous passive motion machine that cradles and moves your leg.
If your bone is fractured in many pieces or your bone is weak, it may take longer to heal, and it may be a longer time before your doctor recommends motion activities.
Once you are allowed to put weight on your leg, it will feel weak, stiff, and unsteady. A rehabilitation or physical therapy plan will be designed to help you regain as much function as possible.
Videos
Related specialties
- ACL Injuries
- Arthroscopic Chondroplasty
- Articular Cartilage Restoration
- Deep Thigh Bruising
- Iliotibial Band Syndrome
- Lateral Collateral Ligament (LCL) Injuries
- MACI
- Medial Collateral Ligament Injuries
- Meniscus Tears
- Muscle Spasms
- Muscle Strains of the Calf
- Partial Knee Replacement
- Patellar Fracture
- Quadriceps Tendon Tear
- Runner's Knee
- Senior Strong
- Shin Splints
- Total Knee Replacement Surgery
