Anterior cervical corpectomy & discectomy
A functioning backbone and spinal column are key to living a long and healthy life. They provide the foundation supporting your body’s limbs and other physical parts. They also play an important role in helping you carry out essential but crucial functions like breathing and waste elimination.
Problems of the backbone and spinal cord should always be taken seriously and treated as soon as possible. One of these conditions is called spinal stenosis. Anterior cervical corpectomy and discectomy can provide relief of associated discomfort and other painful symptoms.
Anatomy
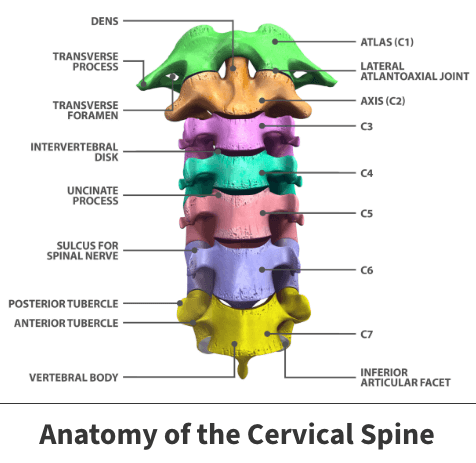
The spine extends from your head all the way down through your back. The portion located in your neck is known as the cervical spine. It is made up of many surrounding physical components, such as vertebrae and intervertebral discs Vertebrae are tiny bones forming to make up the backbone, while discs act as cushions and are located near the vertebra.
About
Over time, vertebra and discs can encounter damage resulting from aging, injury, or bone diseases like osteoporosis. Additionally, malformed structures could eventually lead to a narrowing of the open spaces in your spinal region. If this happens, it places significant pressure on and injures the nerves. This condition is called spinal stenosis.
Causes
Spinal stenosis might result from conditions including:
- Bone overgrowth
- Thickening of ligaments, which are the soft tissues connecting spinal bones
- Immediate traumatic incidents, like excessively forceful physical contact, car accidents, or significant falls
- Herniated discs
- Genetic spinal malformations
Less commonly, stenosis can result from benign or cancerous tumors developing in or around the spine.
Risk factors
Your risk of developing spinal stenosis increases with age. A significant percentage of those diagnosed with the condition are age 50 and older. Injury-producing trauma or degenerative conditions can strike at any age.
Symptoms
You may experience neck discomfort, weakness, numbness, tingling in your arms, legs, hands, or feet, and difficulty maintaining your balance. In the most severe instances, you may also have an inability to control bowel or bladder functions.
Complications
If left untreated, stenosis can progress and potentially result in permanent issues. Some of these include balance issues, limb weakness, the inability to control bowel or bladder functions, mobility issues, chronic pain, and possibly even paralysis.
Diagnosis
Your doctor will confirm the diagnosis using diagnostic imaging tools like a CT scan (computed tomography), MRI (magnetic resonance imaging), or X-rays. They reveal abnormalities like vertebral or disc damage and the development of stenosis.
Anterior cervical corpectomy and discectomy
This procedure involves the removal of damaged or diseased vertebra and discs causing the stenosis and spinal nerve compression. The surgeon enters your neck’s front or anterior region, called the cervical spine.
In most instances, other options are tried before proceeding with surgery. These treatments may include physical therapy and various pain-relieving medications.
Circumstances where surgery is the preferred treatment option
Doctors will usually recommend surgical intervention when:
- Nonsurgical treatments are not effective
- You experience significant pain or disability
- Spinal nerves are compressed, and you experience associated symptoms
- Performing basic tasks prove difficult
Surgery is almost always the preferred treatment option when further disease progression could lead to permanent spinal cord injury.

Treatment
Before the actual anterior cervical corpectomy process begins, you are placed under general anesthesia.
Once sedated, surgeons begin the procedure by making an incision into your neck’s frontal region. Surgeons then remove any damaged vertebra, in addition to the discs attached. This first part of the operation is called decompression because it relieves pressure on associated nerves and other surrounding features.
Once this initial phase is completed, surgeons then work to ensure your spine is stable. This process is known as fusion. The surgical team fuses the open spaces left by removed components using implants. Implants are often made up of either the patient’s bone or donations from a bone bank. Occasionally, surgeons insert implants known as cages, created from synthetic products like ceramic or titanium.
After these implants (commonly known as grafts) are positioned, they are tightened using materials like screws and plates. Over time, grafted and existing bone naturally fuse together.
During the operation’s last phase, surgeons stitch and bandage the incision site.
Recovery
You will typically remain hospitalized for only one night following the procedure. Bandages usually remain on for a week.
Your doctor will schedule a follow-up appointment anywhere from four to six weeks after the operation. During this time, X-rays will be taken to track the healing process. On average, total recovery occurs over a six-to-eight-week period.
Until complete healing is complete, you might need to wear a collar or neck brace to support neck muscles. Additionally, your doctor might recommend that you undergo physical therapy to strengthen your neck and maintain its range of motion.
Until your neck has healed entirely, you should avoid any strenuous activities. Basic but beneficial activities like walking are acceptable.
Videos
Related specialties
- Artificial Disc Replacement (ADR)
- Bone Cement Injection
- Degenerative Disc Disease
- Diffuse Idiopathic Skeletal Hyperostosis (DISH)
- Discectomy
- Discitis Treatment & Information
- Epidural Injections for Spinal Pain
- Foraminotomy
- Interlaminar Implants
- Interlaminar Lumbar Instrumental Fusion: ILIF
- Kyphoplasty (Balloon Vertebroplasty)
- Kyphosis
- Laminectomy: Decompression Surgery
- Lumbar Epidural Steroid Injection
- Lumbar Interbody Fusion (IBF)
- Minimally Invasive Spine Surgery
- Outpatient Spine Surgery
- Pinched Nerve
- Piriformis Syndrome
- Sacroiliac Joint Pain
- Sciatica
- Scoliosis
- Spinal Fusion
- Spondylolisthesis & Spondylolysis
- Vertebroplasty
- Whiplash & Whiplash Associated Disorder (WAD)
