Skin grafts on hands
The skin is an integral part of the hand. This outer layering of cells and tissues protects your fingers, palm, wrist, and the bones, muscles, ligaments, tendons, and blood vessels that make up your hands.
Should your skin sustain any type of severe injury or illness, your hand’s inner workings can be threatened. Such an occurrence could limit your ability to perform basic tasks and, in some cases, make moving your hand and fingers quite challenging. Fortunately, badly damaged skin can be replaced through a surgical process called skin grafting.
Anatomy
Skin comprising the hands is made of several different types. The skin situated between and beneath your fingers is thin and easy to move. The skin on the hand’s bottom (the palm) is thicker and more difficult to move.
About
Severely damaged or diseased skin can pose significant, possibly life-threatening health concerns because it is not capable of protecting the hand’s inner workings from potentially serious invaders, such as bacteria and viruses. Should you face such circumstances, you might be a candidate for skin grafting. Surgeons perform this procedure by using skin from another part of the body to replace injured or diseased tissue.
Issues that may require grafting
Grafting is typically only carried out on severely hurt or sick skin that no other form of treatment either has been or would be effective.
Burns are the most common reason a hand’s skin is grafted. Other problems that might bring about the need for such a skin graft procedure include:
- Infections
- Wounds, such as stab marks, slashes, and animal bites
- Bedsores, like those a bedridden individual might experience
- Significant skin diseases
Additionally, grafting is also conducted for aesthetic purposes to heal blemishes made during surgery to remove various skin-related cancers.

Diagnosis
If your hands sustain significant burns following an emergency such as a fire or chemical accident, your physician will likely recommend you undergo some type of grafting procedure. Failure to immediately fix damaged skin could result in life-threatening infections.
If your damaged skin is the result of chronic sickness or longstanding process of physical breakdown, your doctor is more likely to weigh the pros and cons of undergoing skin grafts. It is important to remember that grafting is a delicate process, often requiring lengthy recovery that comes with no guarantees.
Treatment
Grafting is a serious surgery necessitating appropriate preparation. The process is almost always performed in a hospital setting.
Types of grafting procedures
Usually, the two most commonly performed grafting processes include split-thickness grafts and full-thickness grafts.
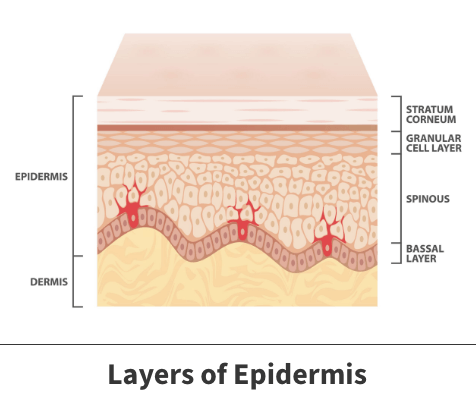
- Split-thickness – During this process, you receive a new outer skin layering known as the epidermis, in addition to a part of the dermis, which is the layer of skin immediately beneath the epidermis.
- Full-thickness – Full-thickness grafts involve replacing the epidermis and dermis in their entirety.
Grafting is a serious surgery necessitating appropriate preparation.
Preparation
Except following emergencies, skin grafts are typically carried out several weeks after your surgeon schedules such procedures.
During the planning stages, you need to disclose any prescription or over-the-counter medications you are taking. Certain drugs, most notably aspirin, can thin your blood and make it difficult to properly clot. This event could be a serious complication during any grafting procedure.
If you smoke cigarettes or use other tobacco-based products, your doctor may ask you to stop using them before the surgery. These products interrupt normal blood flow, which slows down the healing process following your graft.
The procedure itself
Before replacing damaged skin, your physician must first get new skin from another region of your body. Exactly where would-be grafted skin is taken from will depend upon whether you are getting a split-thickness or full-thickness graft.
After the new skin is obtained, the material is transplanted onto the area in need and then carefully and thoroughly dressed, stapled, and stitched together. Your surgeon will also dress and stitch together the donor site to prevent any possible complications, like infections.
Immediately following surgery
The first 36 hours following the graft are often crucial to determining how well the surgery went. Throughout this timeframe, the newly transplanted skin should develop blood vessels and connect to nearby tissues. If these events do not happen, the graft has failed to take, and you might need to undergo another grafting procedure.
Post hospital surgery
Even if your graft holds, you will be asked to follow specific instructions about how to clean and protect your hand correctly. Usually, you should avoid strenuous activities. Furthermore, your physician will continue to watch your progress and let you know when you can return to your regular work and leisure schedule.
Videos
Related specialties
- Basal Joint Surgery
- Carpal Tunnel Syndrome
- De Quervain's Tenosynovitis
- Dislocated Finger
- Distal Radius Fracture (Broken Wrist)
- Dupuytren’s Disease
- Flexor Tendonitis
- Fractured Fingers
- Functional Nerve Transfers of the Hand
- Ganglion Cysts
- Hand & Finger Replantation
- Hand Nerve Decompression
- Nerve Pain
- Peripheral Nerve Surgery (Hand) Revision
- Revascularization of the Hand
- Rheumatoid Arthritis of the Hand
- Sports Wrist & Hand Injuries
- Sprained Wrist
- Sudden Acute Finger, Hand & Wrist Injuries
- Targeted Muscle Reinnervation (TMR)
- Tendon Transfers of the Hand
- Thumb Ulnar Collateral Ligament Injuries
- Trigger Finger
- Ulnar Neuritis
- WALANT (Wide Awake Local Anesthesia No Tourniquet)
- Wrist Arthroscopy
- Wrist Fractures
- Wrist Tendonitis
