Ankle cartilage damage
Your ankles are extremely important. They enable you to move your feet and perform activities such as walking, running, standing, jumping, and turning your legs.
The ankles are strong and capable of handling a significant amount of wear. However, constantly bearing the body’s weight, in addition to events like age, overuse, traumatic accidents, or participation in competitive athletics, can quickly or gradually result in weakening and the development of various physical conditions. One such condition is articular cartilage damage.
Anatomy
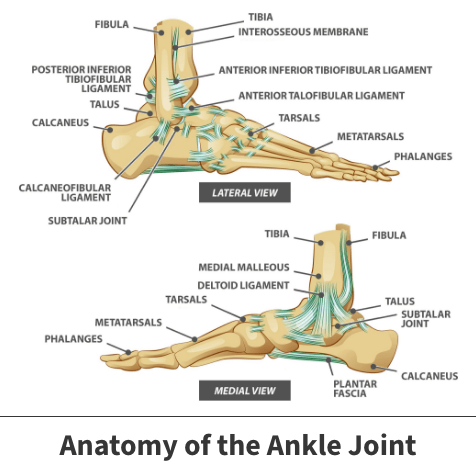
Articular cartilage is a soft tissue protecting the parts of bones where they fit into joints. The ankle is one of the body’s major joints and connects three important structures: the leg bones (known as the tibia and fibula) and the foot bone (the talus).
Cartilage serves several functions. It protects bones from injury and also prevents joint friction.
About
Articular cartilage damage can cause discomfort and disrupt the normal operation and movement of surrounding bones, muscles, and other soft tissues.
Causes for cartilage deterioration
Several underlying factors can contribute to articular cartilage damage.
The most notable cause is age. Cartilage tends to weaken and deteriorate as you age. Furthermore, this problem is often worsened because articular cartilage has limited or no blood supply, which is necessary for the healing process. Damaged articular cartilage cannot repair itself.
Another notable cause is traumatic injury. A sudden fall or car accident can result in immediate and direct cartilage injury.
Other moderate to severe ankle injuries can also result in cartilage damage. Doctors often discover articular cartilage issues when diagnosing other problems, including dislocations, bone breakages, and ligament sprains.
Risk factors
Naturally, your risk of developing age-related cartilage deterioration is greater if you are older. If you compete in competitive contact sports, participate in activities placing significant pressure on your feet, or work in a profession requiring you to stand or continually turn your legs and feet, your chances increase.
Symptoms
The symptoms you feel may vary depending on how bad your injury is. That said, common occurrences include:
- Ankle stiffness
- Pain
- Redness
- Tenderness
- Swelling
- A popping or clicking sensation coming from your affected ankle
These symptoms might intensify when you stand, place weight on your ankle or you engage in any type of movement. Additionally, in more serious cases, your joint may lock, which could limit your mobility. You could also experience instability or the feeling that your ankle is about to give out.
Complications
If left untreated, articular cartilage damage will likely worsen, leading to more intense pain, mobility problems, and other related symptoms. Furthermore, as cartilage gradually weakens, your ankle bones receive less and less protection. Such events can place these physical structures at an increased risk of fractures and ailments like osteoarthritis.

Diagnosis
Your physician will likely first request that you undergo a weight-bearing X-ray. This means that you will stand when the X-ray is taken. This scan enables your doctor to view the ankle’s internal structural condition.
You may need more advanced imaging devices like magnetic resonance imaging (M.R.I. scans). Articular cartilage is also referred to as hyaline cartilage. Unfortunately, this type of material does not contain calcium, occasionally making injuries more challenging to identify on X-rays.
Treatment
Orthopedic doctors typically place articular cartilage injuries into categories ranging in severity from one to four, using the Outerbridge classification of cartilage damage. These grades are based on the appearance of the articular cartilage when seen at arthroscopy.
- Grade 0 – Normal cartilage
- Grade 1 – Cartilage softening and swelling
- Grade 2 – Partial-thickness loss with fissures on the surface that do not reach subchondral bone or exceed 1.5 cm in diameter
- Grade 3 – Fissuring to the level of subchondral bone in an area with a diameter more than 1.5 cm
- Grade 4 – Exposed subchondral bone
Treatment may not always need surgery. Naturally, less severe damage will likely need less aggressive therapy.
Other factors may play into the type of treatment you receive, such as:
- Your age
- Your physical condition
- If you have any underlying illnesses
- If any other ankle injuries are present
- Your height
- Your weight
Often athletes will undergo more advanced treatment geared towards helping them begin the recovery process quicker.
Nonsurgical options
In uncomplicated, mild cases, simple home remedies can produce improvement. One commonly used therapeutic effort is called the RICE technique.
R.I.C.E. is short for Resting the injured ankle, applying Ice to the injured area, Compressing the ankle to prevent the joint from exposure or further injury, and keeping the structure Elevated.
Additional non-surgical therapies might include placing your ankle inside a cast to prevent unnecessary movement and the use of over-the-counter or prescription pain-relieving or anti-inflammatory medications.
Surgical interventions
Mild to moderate occurrences are often corrected using arthroscopic articular cartilage repair.
Surgeons perform this procedure by inserting a small camera-operated device called an arthroscope into your ankle. The pictures generated from the arthroscope enable the surgeon to remove or repair damaged cartilage using tiny instruments.
Doctors prefer using arthroscopic repair because it is considered minimally invasive. This means the operation does not need large incisions or lead to significant scarring after the procedure is completed.
More serious cases may need more aggressive procedures like microfracture surgery and cartilage transplantation.
Following an operation, you will likely be required to remain off your ankle for at least a month or more. As your ankle gradually heals, you will need to undergo physical therapy – a collection of exercises designed to help your ankle regain strength and mobility.
Videos
Related specialties
- Achilles Calcific Tendinitis
- Achilles Tendon Rupture
- Achilles Tendonitis
- Ankle Fracture Surgery
- Ankle Fractures (Broken Ankle)
- Ankle Fusion Surgery
- Arthroscopy of the Ankle
- Bunions
- Charcot Joint
- Common Foot Fractures in Athletes
- Foot Stress Fractures
- Hallux Rigidus Surgery - Cheilectomy
- Hammer Toe
- High Ankle Sprain (Syndesmosis Ligament Injury)
- Intraarticular Calcaneal Fracture
- Lisfranc Injuries
- Mallet, Hammer & Claw Toes
- Metatarsalgia
- Neuromas (Foot)
- Plantar Fasciitis
- Sprained Ankle
- Total Ankle Replacement
- Turf Toe
