Achilles Tendonitis
OVERVIEW
The Achilles tendon, also known as the calcaneal tendon, is a tough, fibrous band of tissue that connects the calf muscle to the heel bone (calcaneus). Achilles tendonitis is a common condition that occurs when the large tendon that runs down the back of your lower leg becomes irritated and inflamed. The severity of the tendonitis is a major factor in the type of treatment you will receive. Regardless of the kind of treatment, most people make a full recovery in approximately 12 months.
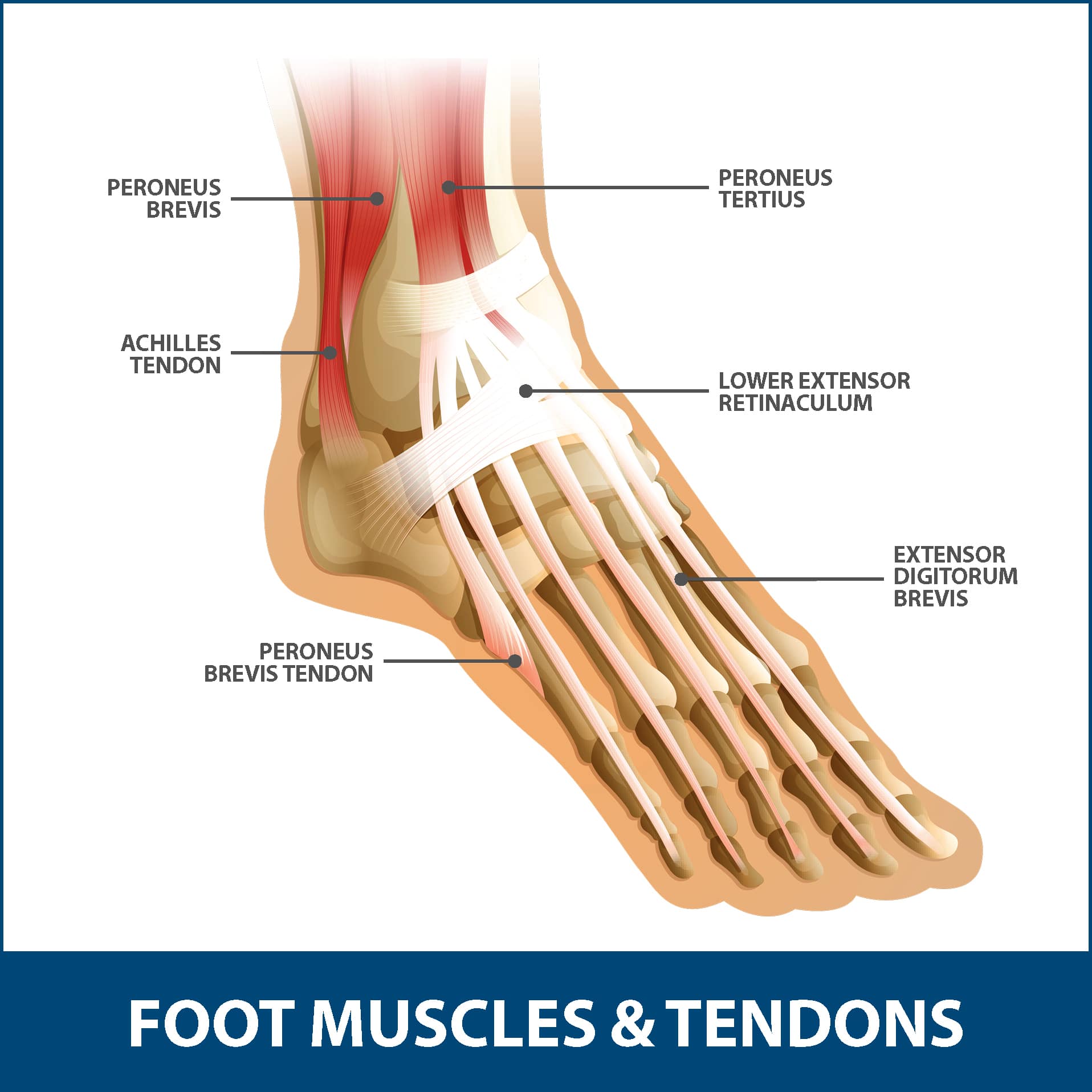
ANATOMY
The Achilles tendon, also known as the calcaneal tendon, is a tough, fibrous band of tissue that connects the calf muscle to the heel bone (calcaneus). When the calf muscles flex, the Achilles tendon pulls on the heel, allowing us to walk, run, climb stairs, jump, and stand on the tip of our toes. It is both the strongest and largest tendon in the entire body. While it may be the strongest, it is also vulnerable to injury, due to the high tensions placed on it and its limited blood supply. The tearing of the Achilles tendon is when the tendon tears, resulting in the separation of the tendon fibers. When this occurs, the tendon can no longer perform its normal functions.
DESCRIPTION
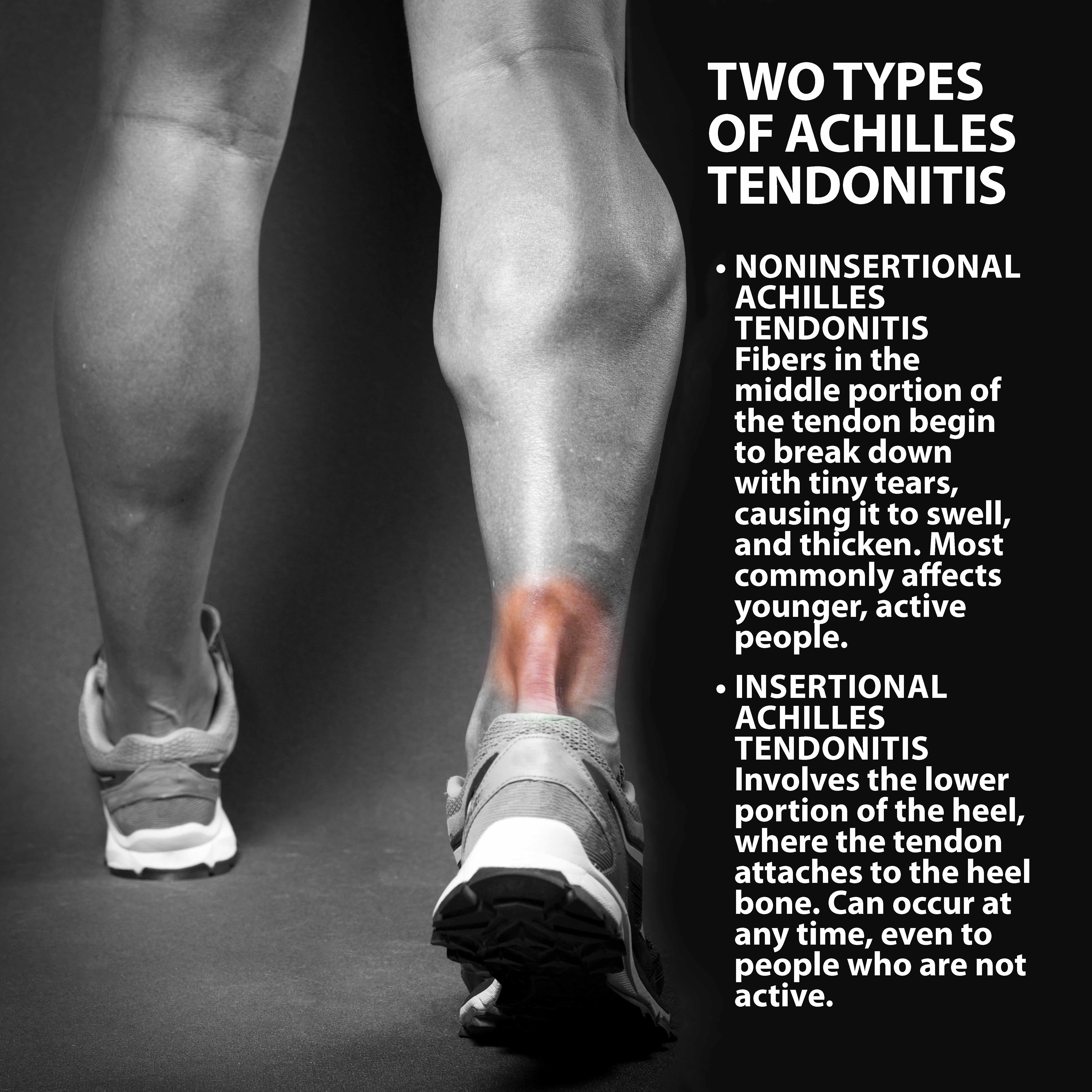
Achilles tendonitis is a common condition that occurs when the large tendon that runs down the back of your lower leg becomes irritated and inflamed. Although the Achilles tendon can withstand high stresses from running and jumping, it is also prone to tendonitis, a condition associated with degeneration and overuse. There are two different types of Achilles tendonitis, noninsertional and insertional:
- Noninsertional Achilles Tendonitis. Fibers in the middle part of the tendon begin to break down with tiny tears, causing the tendon to swell and thicken. This type of tendonitis most commonly affects younger, active people.
- Insertional Achilles Tendonitis involves the lower part of the heel, where the tendon attaches to the heel bone. This type of tendonitis can occur at any time, even to people who are not active. Extra bone growth (bone spurs) often form with insertional Achilles tendonitis.
In both types, damaged tendon fibers may also harden (calcify).
SYMPTOMS
Common symptoms of Achilles tendonitis include:
- Severe pain the day after exercising
- Thickening of the tendon
- Pain and stiffness along the Achilles tendon in the morning.
- Pain along the tendon or back of the heel that worsens with activity.
- Bone spurs (only with insertional tendonitis).
- Swelling that is present all the time, and gets worse throughout the day with activity.

DIAGNOSIS
Your Florida Orthopaedic Institute physician will take a look at your symptoms, and examine your foot and ankle, keeping an eye out for:
- Swelling along the Achilles tendon or at the back of your heel.
- Bony spurs at the lower part of the tendon at the back of your heel (insertional tendonitis).
- Thickening or enlargement of the Achilles tendon.
- The point of greatest tenderness.
- Limited range of motion in your ankle—specifically, a decreased ability to flex your foot.
- Pain at the back of your heel at the lower part of the tendon (insertional tendonitis).
- Pain in the middle of the tendon (noninsertional tendonitis).
Your physician may also order some tests to make sure that your symptoms are caused by Achilles tendonitis and not something else. These tests include:
- X-rays. This test can show whether the lower part of the Achilles tendon has calcified, or become hardened. This calcification proves that you have insertional Achilles tendonitis.
- Magnetic Resonance Imaging (MRI). This test is not actually necessary to diagnose Achilles tendonitis but it does help with planning surgery. An MRI scan can show the severity of the damage to the Achilles tendon. If surgery is needed, your doctor will select the procedure based on the amount of tendon damage.
TREATMENT OVERVIEW
Nonsurgical treatments are in most cases, recommended first. If they are unsuccessful or if the tendonitis is severe, then surgical treatments are recommended. There are many different options for each type of treatment that will help you have a smooth recovery.
NONSURGICAL TREATMENT
Non-surgical treatment, in most cases, will provide pain relief, though it may take a few months for symptoms to subside. The length of your recovery is heavily dependent on the severity of your injury. The following non-surgical treatments help expedite the healing process and ensure your safety:
- Rest. The first step to reducing pain is to allow yourself to rest by stopping all activities that make the pain worse. Switch to low-impact actives that put less stress on your Achilles tendon.
- Ice. Icing the area of pain can help with pain management and can be done throughout the day. This can be done for up to 20 minutes and should be stopped if the skin becomes numb
- Medication. Non-steroidal anti-inflammatory medication such as ibuprofen (Advil, Motrin) and naproxen (Aleve) help reduce swelling and pain.
- Exercise. Exercises that strengthen the calf muscles can reduce stress on the Achilles tendon.
- Physical Therapy.
- Cortisone injections. Cortisone is a type of steroid that works as a powerful anti-inflammatory used to help control the swelling caused by Achilles tendonitis.
- Extracorporeal shockwave therapy (ESWT). High-energy shockwave impulses stimulate the healing process in damaged tendon tissue.
SURGICAL TREATMENT
Surgery is only considered if the tendonitis does not improve after 6 months of non-surgical treatments. The specific type of surgery depends on the location of the tendonitis and the amount of damage to the tendon.
- Gastrocnemius recession. This is a surgical lengthening of the calf muscles (gastrocnemius muscles). Because tight calf muscles place increased stress on the Achilles tendon, this procedure is useful for patients who still have difficulty flexing their feet, even after consistently stretching the muscle. During this procedure, one of the two muscles that make up the calf is lengthened to increase the motion of the ankle.
- Debridement and repair. This procedure is only used when less than half of the tendon is damaged. The goal of this operation is to remove the damaged part of the Achilles tendon, and repair the remaining pieces of the tendon with sutures, or stitches. If you have insertional tendonitis, then bone spurs are also removed at the same time.
- Debridement with tendon transfer. This procedure is only used when more than half of the tendon is damaged. The tendon that helps the big toe point down is moved to the heel bone to add strength to the damaged tendon. Depending on the extent of damage to the tendon, some patients may not be able to return to competitive sports or running.
NEXT STEPS
Most patients have good results from surgery, and recovery usually lasts about 12 months. The greater the amount of tendon that is involved, the longer the recovery period, and the less likely a patient will be able to return to sports activity. Physical therapy will also be required to ensure a full recovery. Talk to your Florida Orthopaedic Institute physician if you have further questions.
Areas of Focus
- Foot, Ankle & Lower Leg
- Achilles Tendinitis - Achilles Insertional Calcific Tendinopathy (ACIT)
- Achilles Tendon Rupture
- Achilles Tendonitis
- Ankle Fracture Surgery
- Ankle Fractures (Broken Ankle)
- Ankle Fusion Surgery
- Arthroscopic Articular Cartilage Repair
- Arthroscopy Of the Ankle
- Bunions
- Charcot Joint
- Common Foot Fractures in Athletes
- Foot Stress Fractures
- Hallux Rigidus Surgery - Cheilectomy
- Hammer Toe
- High Ankle Sprain (Syndesmosis Ligament Injury)
- Intraarticular Calcaneal Fracture
- Lisfranc Injuries
- Mallet, Hammer & Claw Toes
- Metatarsalgia
- Morton’s Neuroma
- Neuromas (Foot)
- Orthopedic Physician Or A Podiatrist? Definition of a Podiatrist
- Plantar Fasciitis
- Sports Foot Injuries
- Sprained Ankle
- Total Ankle Replacement
- Turf Toe
Specialties
- AC Joint Injuries
- Achilles Tendinitis - Achilles Insertional Calcific Tendinopathy (ACIT)
- Achilles Tendon Rupture
- Achilles Tendonitis
- ACL Injuries
- Ankle Fracture Surgery
- Ankle Fractures (Broken Ankle)
- Ankle Fusion Surgery
- Anterior Cervical Corpectomy & Discectomy
- Arthroscopic Articular Cartilage Repair
- Arthroscopic Chondroplasty
- Arthroscopic Debridement of the Elbow
- Arthroscopy Of the Ankle
- Articular Cartilage Restoration
- Artificial Disk Replacement (ADR)
- Aspiration of the Olecranon Bursa - Fluid In Elbow
- Atraumatic Shoulder Instability
- Avascular Necrosis (Osteonecrosis)
- Bankart Repair
- Basal Joint Surgery
- Bicep Tendon Tear
- Bicep Tenodesis
- Bone Cement Injection
- Bone Growth Stimulation
- Bone Health Clinic
- Broken Collarbone
- Bunions
- Bursitis of the Shoulder (Subacromial Bursitis)
- Calcific Tendinitis of the Shoulder
- Carpal Tunnel Syndrome
- Charcot Joint
- Chiropractic
- Clavicle Fractures
- Colles’ Fractures (Broken Wrist)
- Common Foot Fractures in Athletes
- Community Outreach
- Cubital Tunnel Syndrome
- De Quervain's Tenosynovitis
- Deep Thigh Bruising
- Degenerative Disk Disease
- Diffuse Idiopathic Skeletal Hyperostosis (DISH)
- Discectomy
- Discitis Treatment & Information
- Dislocated Shoulder
- Dupuytren’s Disease
- Elbow
- Elbow Bursitis
- Elbow Injuries & Inner Elbow Pain in Throwing Athletes
- Epidural Injections for Spinal Pain
- Finger Dislocation
- Flexor Tendonitis
- Foot Stress Fractures
- Foot, Ankle & Lower Leg
- Foraminotomy
- Fractured Fingers
- Fractures Of The Shoulder Blade (Scapula)
- Fractures Of The Tibial Spine
- Functional Nerve Transfers of The Hand
- Ganglion Cysts
- General Orthopedics
- Glenoid Labrum Tear
- Golfer's Elbow
- Groin Strains and Pulls
- Growth Plate Injuries Of The Elbow
- Hallux Rigidus Surgery - Cheilectomy
- Hammer Toe
- Hamstring Injuries
- Hand & Finger Replantation
- Hand & Wrist
- Hand Nerve Decompression
- Hand Skin Grafts
- Hand, Wrist, Elbow & Shoulder
- Heat Injury/Heat Prostration
- High Ankle Sprain (Syndesmosis Ligament Injury)
- Hip & Thigh
- Hip Arthroscopy
- Hip Dislocation
- Hip Flexor Strains
- Hip Fractures
- Hip Hemiarthroplasty
- Hip Impingement Labral Tears
- Hip Muscle Strains
- Hip Pointers and Trochanteric Bursitis
- Hyperextension Injury of the Elbow
- Iliopsoas Tenotomy
- Iliotibial Band Syndrome
- Impingement Syndrome of the Shoulder
- Interlaminar Implants
- Interlaminar Lumbar Instrumental Fusion: ILIF
- Interventional Pain Management
- Interventional Spine
- Intraarticular Calcaneal Fracture
- Joint Replacement
- Knee & Leg
- Kyphoplasty (Balloon Vertebroplasty)
- Kyphosis
- Labral Tears Of The Hip (Acetabular Labrum Tears)
- Laminectomy: Decompression Surgery
- Lateral Collateral Ligament (LCL) Injuries
- Lisfranc Injuries
- Little League Shoulder
- LITTLE LEAGUER'S ELBOW (MEDIAL APOPHYSITIS)
- Lumbar Epidural Steroid Injection
- Lumbar Interbody Fusion (IBF)
- MACI
- Mallet, Hammer & Claw Toes
- Medial Collateral Ligament Injuries
- Meniscus Tears
- Metatarsalgia
- Minimally Invasive Spine Surgery
- Morton’s Neuroma
- Muscle Spasms
- Muscle Strains of The Calf
- Nerve Pain
- Neuromas (Foot)
- Neurosurgery
- Olecranon Stress Fractures
- Orthopaedic Total Wellness
- Orthopaedic Trauma
- Orthopedic Physician Or A Podiatrist? Definition of a Podiatrist
- Osteoarthritis of the Hip
- Osteoporosis
- Outpatient Spine Surgery
- Partial Knee Replacement
- Patellar Fracture
- Pelvic Ring Fractures
- Peripheral Nerve Surgery (Hand) Revision
- Pinched Nerve
- Piriformis Syndrome
- Piriformis Syndrome
- Plantar Fasciitis
- Plastic Surgery
- Podiatry
- Primary Care Sports Medicine
- Quadriceps Tendon Tear
- Radial Tunnel Syndrome (Entrapment of the Radial Nerve)
- Revascularization of the Hand
- Reverse Total Shoulder Replacement
- Rheumatoid Arthritis (RA) of the Shoulder
- Rheumatoid Arthritis Of The Hand
- Robotics
- Rotator Cuff Tears
- Runner's Knee
- Sacroiliac Joint Pain
- Sciatica
- Scoliosis
- Senior Strong
- Shin Splints
- Shoulder
- Shoulder Arthritis
- Shoulder Arthroscopy
- Shoulder Injury: Pain In The Overhead Athlete
- Shoulder Replacement
- Shoulder Separations
- Shoulder Socket Fracture (Glenoid Fracture)
- SLAP Tears & Repairs
- Spinal Fusion
- Spine
- Spondylolisthesis and Spondylolysis
- Sports Foot Injuries
- Sports Hernias (Athletic Pubalgia)
- Sports Medicine
- Sports Wrist and Hand Injuries
- Sprained Ankle
- Sprained Wrist Symptoms and Treatment
- Subacromial Decompression
- Sudden (Acute) Finger, Hand & Wrist Injuries
- Targeted Muscle Reinnervation (TMR)
- Tendon Transfers of The Hand
- Tennis Elbow Treatment
- Thigh Fractures
- Thigh Muscle Strains
- Thumb Ulnar Collateral Ligament Injuries
- Total Ankle Replacement
- Total Hip Arthroplasty
- Total Hip Replacement - Anterior Approach
- Total Knee Replacement Surgery
- Trapezius Strain (Muscle Strain of The Upper Back)
- Traumatic Shoulder Instability
- Tricep Pain & Tendonitis
- Trigger Finger
- Turf Toe
- UCL (Ulnar Collateral Ligament) Injuries
- Ulnar Neuritis
- Valgus Extension Overload
- Vertebroplasty
- WALANT (Wide Awake Local Anesthesia No Tourniquet)
- Whiplash and Whiplash Associated Disorder (WAD)
- Wound Care
- Wrist Arthroscopy
- Wrist Fractures
- Wrist Tendonitis
Services
- Physical Medicine & Rehabilitation
- Physical Therapy
- Primary Care Sports Medicine
- PROMs (Patient-Reported Outcome Measures)
- Same-Day Orthopaedic Appointments Now Available
- Sports Medicine
- Sports-Related Concussion Treatment
- Telehealth Page
- Telemedicine
- Workers' Compensation
- Workers' Compensation Dispensary
- X-Ray
