Stress Fracture in the Foot
Overview
Your feet are two of your most important physical features. Without them, you could not stand up, walk, run, or carry out any other movement requiring your legs. Your feet also help you maintain your balance.
These heavy responsibilities and continued use leave feet more likely to sustain injury. A common concern is a stress fracture.
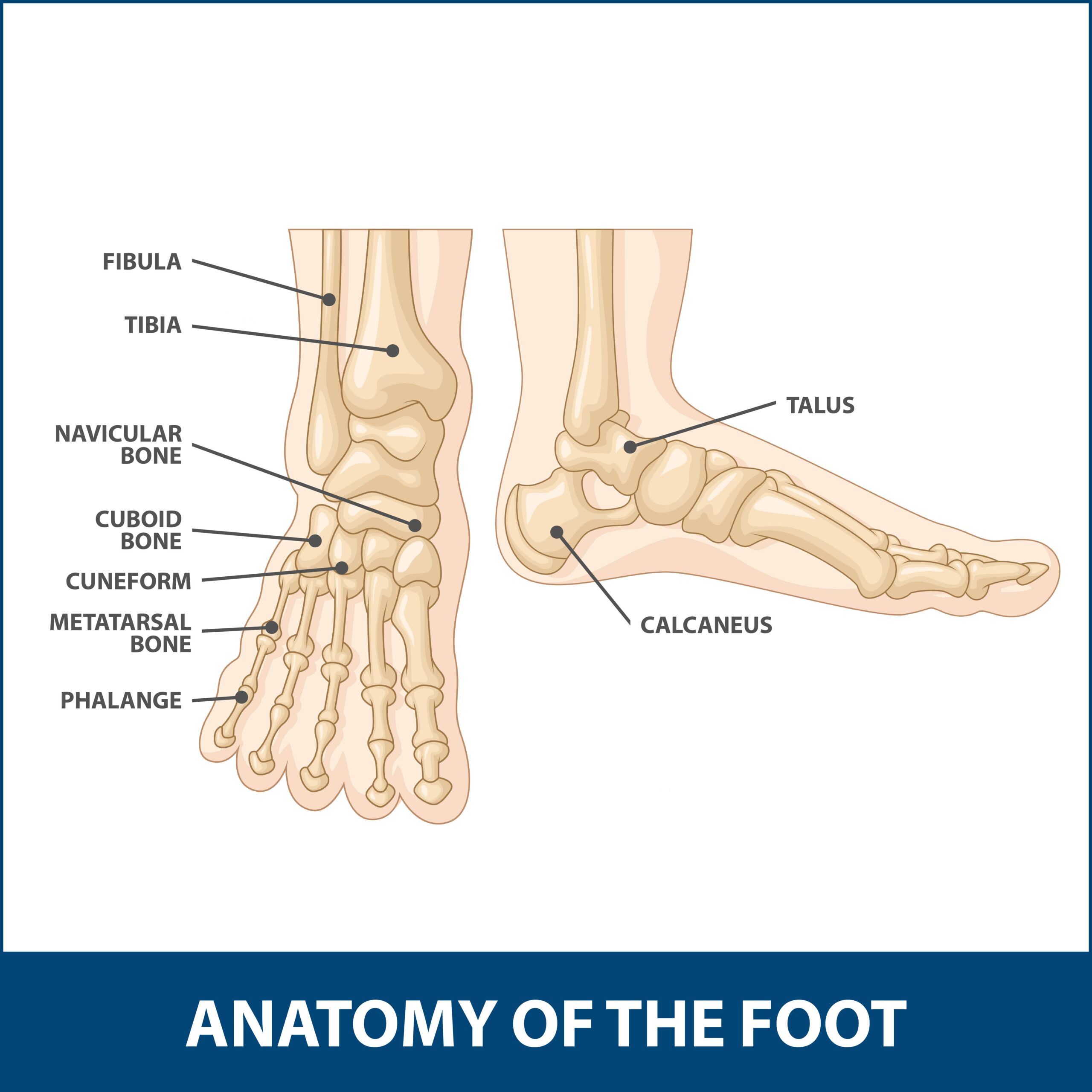
Anatomy
The feet are made up of many features. Among them are several relatively large as well as very small bones. Specific foot bones include the following:
- Front Foot Bones – These bones (metatarsals) are long and thin structures in the foot’s top and front. They are crucial in one’s ability to walk or bend their feet forward. These bones most commonly experience stress fractures.
- Heel Bone – Medically, the heel bone is called the calcaneus. This is the second most common area where foot stress fractures are seen.
- Foot Ball Bones – These bones are positioned in the ball of the foot, not far from the big toe. These bones provide support for the big toe and enable people to stand, walk, and bend their feet.
- Middle Foot Bone – The navicular is a key middle foot bone. It allows people to bear weight and take steps.
- Middle Heel Bone – The middle heel bone is known as the talus. This feature provides added support for the heel and helps keep your feet balanced.
Description
Foot stress fractures happen when a repeated strain, acute injuries, or disease create tiny cracks within any of the previously mentioned bones.
Causes
Stress fractures can result from several different causes, including:
- Repeated movements.
- Quickly increasing one’s activity levels.
- Poor exercise techniques.
- Exercising on different surfaces.
- Bone insufficiency.
- Using the wrong equipment.
- Acute injury.
Most people move their feet continually. Over time, repetitive motions strain bones and might eventually weaken the structures to a point where they might develop stress fractures.
The most common cause of foot stress fractures is a sudden increase in physical activity. For example, someone engaging in a light exercise program might shift to a more intense workout. This may not give the body time to adjust and leaves it more likely to develop injuries like stress fractures.
Having poor posture or not positioning one’s feet correctly during actions like running can increase your chances of experiencing stress fractures. This is because improper techniques force the feet to bear weight more than they typically should and move at odd angles.
When an individual usually works out on a specific surface, their body grows accustomed to it. Suddenly training on a new or uneven surface could heighten one’s risk for stress fractures because the body is not yet used to performing on that material.
Certain medications or diseases like osteoporosis can weaken bones. As such conditions progress, stress fractures can eventually emerge.
Foot stress fractures may also result from using the wrong equipment when exercising. For example, wearing worn, poorly fitting, or inappropriate sneakers or shoes could increase one’s risk of foot injuries.
Sudden events like car accidents, falls, or contact when participating in physical sporting contests could prove problematic.

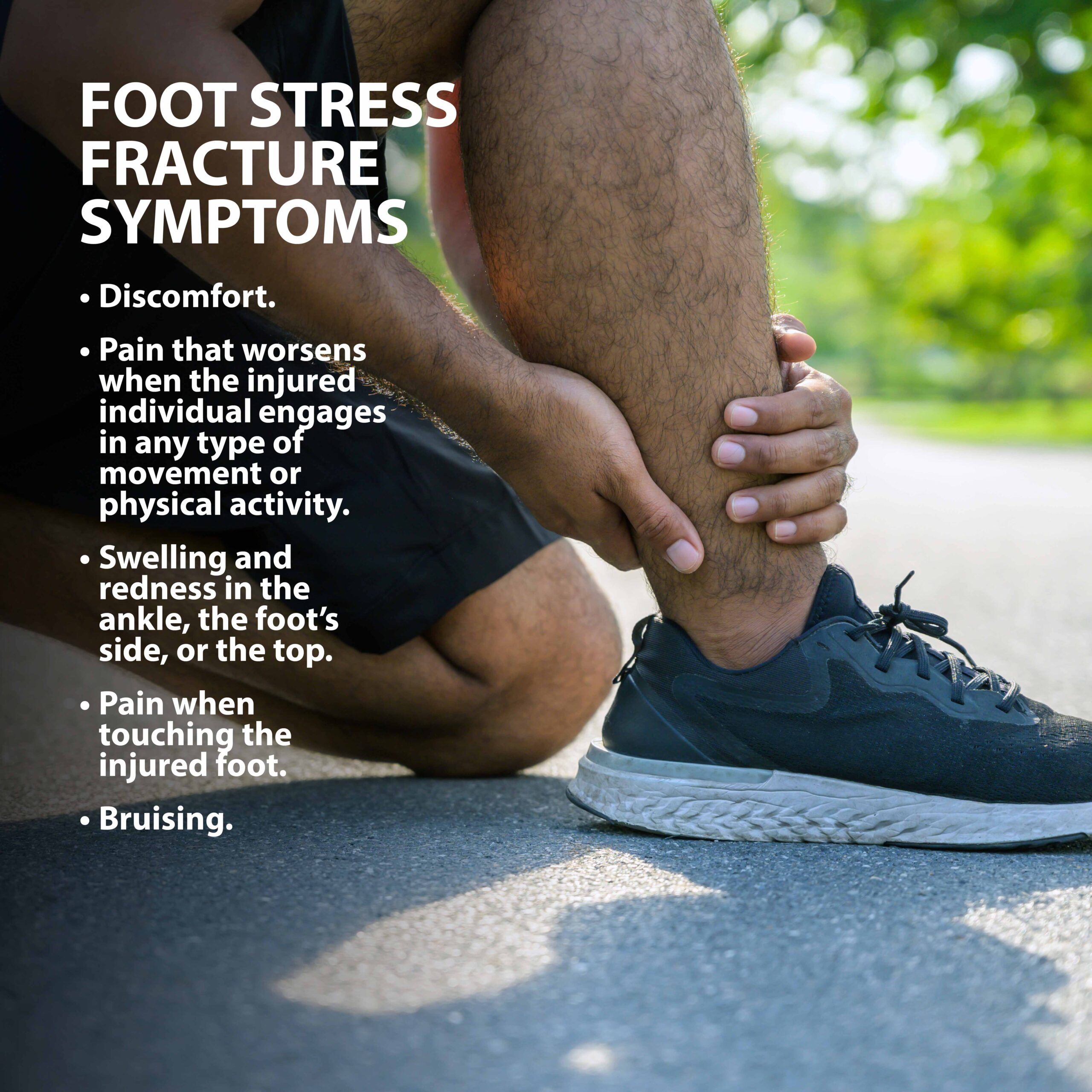
Symptoms
Symptoms may differ depending on the specific location where the stress fracture took place. Such injuries often produce common occurrences such as:
- Discomfort.
- Pain that worsens when the injured individual engages in any type of movement or physical activity.
- Swelling and redness in the ankle, the foot’s side, or the top.
- Pain when touching the injured foot.
- Bruising.
In certain instances, persons with foot stress fractures might also experience problems standing or walking.
Complications
If not diagnosed and treated as soon as possible, stress fractures could grow into larger fractures causing more serious symptoms and requiring more aggressive treatment. Worsening stress fractures could negatively impact other parts of the foot, leaving them at greater risk of developing injury or even permanent disability.
Diagnosis
When an examining doctor believes a patient might have a stress fracture, they will likely ask them several questions about when their pain began, if any movements worsen the discomfort, and their professional and leisure activities.
Doctors will then look closely at the injured foot to check for any irregularities. They might press against the affected area and ask the patient to move or stretch the foot. This helps determine the patient’s range of motion and pain tolerance.
Individuals might also need to undergo some type of internal imaging test. Diagnostic equipment like X-rays and MRIs (Magnetic Resonance Imaging) can reveal the presence of stress fractures or other bone-related problems.
Physicians might also order blood tests to measure if patients lack appropriate levels of nutrients such as calcium and Vitamin D. Insufficient amounts of either can threaten bone strength and health.
Treatment Overview
Home treatment and rest will bring about improvement over time. Certain cases might need surgery.
Non-Surgical Treatment Options
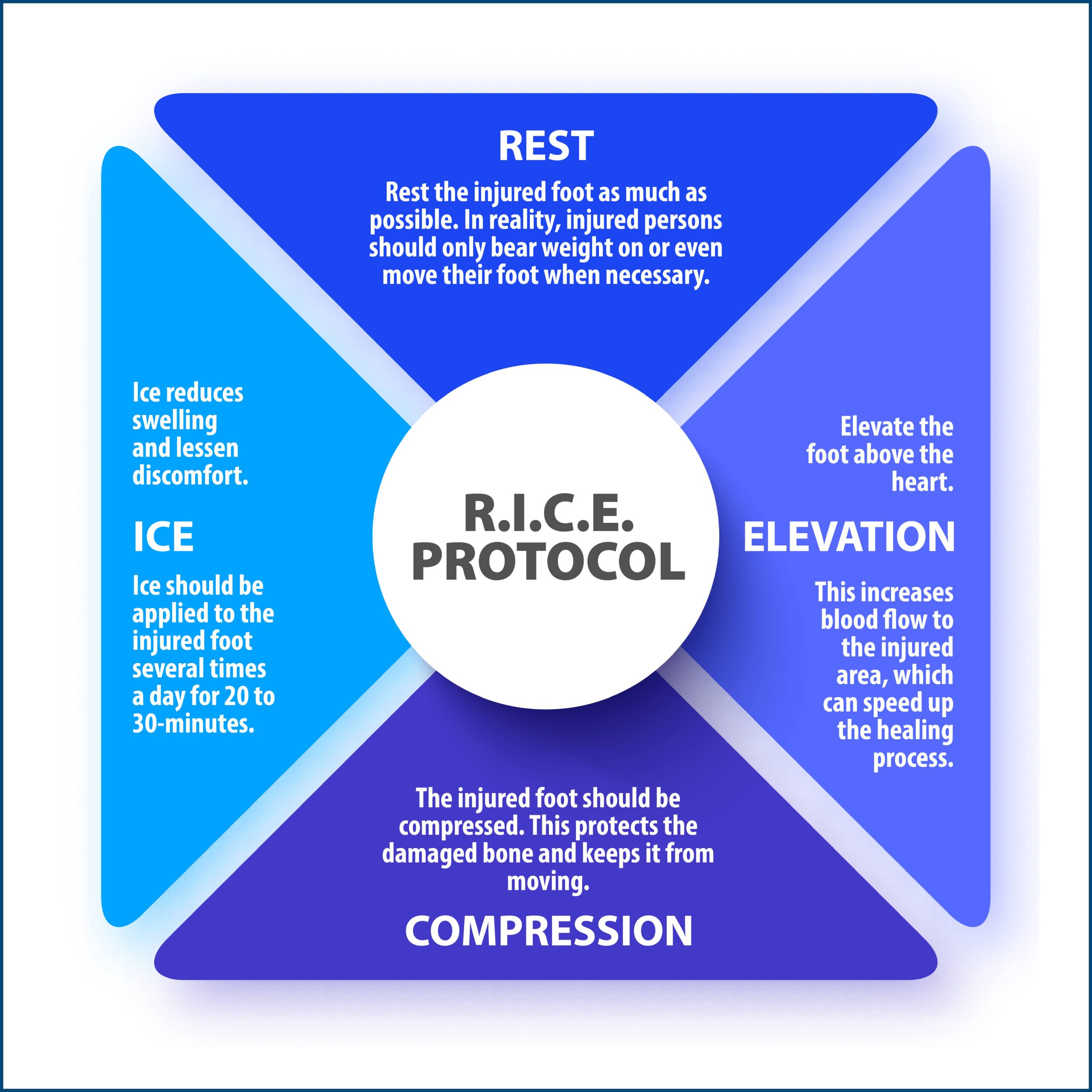
Those diagnosed with or believe that they might have a foot stress fracture are urged to follow a first aid protocol abbreviated as RICE. This stands for:
- Rest – Rest the injured foot as much as possible. In reality, injured persons should only bear weight on or even move their foot when necessary.
- Ice – Ice packets or compresses should be applied to the injured foot several times a day at 20 to 30-minute intervals. Ice reduces swelling and lessen discomfort.
- Compression – The injured foot should be compressed. This protects the damaged bone and keeps it from moving.
- Elevation – Elevate the foot above the heart. This increases blood flow to the injured area, which can speed up the healing process.
Besides the RICE protocol, injured persons can wear protective footwear like special shoes or orthotic devices and place the wounded foot inside a cast.
Surgical Procedures
A small percentage of foot stress fractures will need surgery. This involves inserting metal fasteners into the bone to fuse the injured structure.
Recovery
Everyone heals at their own given pace. On average, foot stress fractures need anywhere from six to eight weeks to heal completely. If complications like limited blood supply to an injured foot or cases where breakages occurred because of weakened bones, healing can take longer.
Prevention
It might be difficult to prevent certain occurrences. You can lessen your risk by using preventative efforts, including:
- A diet containing enough bone-building nutrients like calcium and Vitamin D.
- Engaging in proper workout techniques like stretching.
- Practicing proper posture.
- Wearing the correct footwear when taking part in athletic activities.
Above all, those experiencing any pain or other symptoms potentially associated with a stress fracture are urged to stop physical activities and seek medical attention immediately.
Next Steps
Anyone diagnosed with a foot stress fracture or experiencing associated symptoms is encouraged to contact us. Contact your Florida Orthopaedic Institute physician today.
Areas of Focus
- Foot, Ankle & Lower Leg
- Achilles Tendinitis - Achilles Insertional Calcific Tendinopathy (ACIT)
- Achilles Tendon Rupture
- Achilles Tendonitis
- Ankle Fracture Surgery
- Ankle Fractures (Broken Ankle)
- Ankle Fusion Surgery
- Arthroscopic Articular Cartilage Repair
- Arthroscopy Of the Ankle
- Bunions
- Charcot Joint
- Common Foot Fractures in Athletes
- Foot Stress Fractures
- Hallux Rigidus Surgery - Cheilectomy
- Hammer Toe
- High Ankle Sprain (Syndesmosis Ligament Injury)
- Intraarticular Calcaneal Fracture
- Lisfranc Injuries
- Mallet, Hammer & Claw Toes
- Metatarsalgia
- Morton’s Neuroma
- Neuromas (Foot)
- Orthopedic Physician Or A Podiatrist? Definition of a Podiatrist
- Plantar Fasciitis
- Sports Foot Injuries
- Sprained Ankle
- Total Ankle Replacement
- Turf Toe
The following Florida Orthopaedic Institute physicians specialize in Foot Stress Fractures:
Specialties
- AC Joint Injuries
- Achilles Tendinitis - Achilles Insertional Calcific Tendinopathy (ACIT)
- Achilles Tendon Rupture
- Achilles Tendonitis
- ACL Injuries
- Ankle Fracture Surgery
- Ankle Fractures (Broken Ankle)
- Ankle Fusion Surgery
- Anterior Cervical Corpectomy & Discectomy
- Arthroscopic Articular Cartilage Repair
- Arthroscopic Chondroplasty
- Arthroscopic Debridement of the Elbow
- Arthroscopy Of the Ankle
- Articular Cartilage Restoration
- Artificial Disk Replacement (ADR)
- Aspiration of the Olecranon Bursa - Fluid In Elbow
- Atraumatic Shoulder Instability
- Avascular Necrosis (Osteonecrosis)
- Bankart Repair
- Basal Joint Surgery
- Bicep Tendon Tear
- Bicep Tenodesis
- Bone Cement Injection
- Bone Growth Stimulation
- Bone Health Clinic
- Broken Collarbone
- Bunions
- Bursitis of the Shoulder (Subacromial Bursitis)
- Calcific Tendinitis of the Shoulder
- Carpal Tunnel Syndrome
- Charcot Joint
- Chiropractic
- Clavicle Fractures
- Colles’ Fractures (Broken Wrist)
- Common Foot Fractures in Athletes
- Community Outreach
- Cubital Tunnel Syndrome
- De Quervain's Tenosynovitis
- Deep Thigh Bruising
- Degenerative Disk Disease
- Diffuse Idiopathic Skeletal Hyperostosis (DISH)
- Discectomy
- Discitis Treatment & Information
- Dislocated Shoulder
- Dupuytren’s Disease
- Elbow
- Elbow Bursitis
- Elbow Injuries & Inner Elbow Pain in Throwing Athletes
- Epidural Injections for Spinal Pain
- Finger Dislocation
- Flexor Tendonitis
- Foot Stress Fractures
- Foot, Ankle & Lower Leg
- Foraminotomy
- Fractured Fingers
- Fractures Of The Shoulder Blade (Scapula)
- Fractures Of The Tibial Spine
- Functional Nerve Transfers of The Hand
- Ganglion Cysts
- General Orthopedics
- Glenoid Labrum Tear
- Golfer's Elbow
- Groin Strains and Pulls
- Growth Plate Injuries Of The Elbow
- Hallux Rigidus Surgery - Cheilectomy
- Hammer Toe
- Hamstring Injuries
- Hand & Finger Replantation
- Hand & Wrist
- Hand Nerve Decompression
- Hand Skin Grafts
- Hand, Wrist, Elbow & Shoulder
- Heat Injury/Heat Prostration
- High Ankle Sprain (Syndesmosis Ligament Injury)
- Hip & Thigh
- Hip Arthroscopy
- Hip Dislocation
- Hip Flexor Strains
- Hip Fractures
- Hip Hemiarthroplasty
- Hip Impingement Labral Tears
- Hip Muscle Strains
- Hip Pointers and Trochanteric Bursitis
- Hyperextension Injury of the Elbow
- Iliopsoas Tenotomy
- Iliotibial Band Syndrome
- Impingement Syndrome of the Shoulder
- Interlaminar Implants
- Interlaminar Lumbar Instrumental Fusion: ILIF
- Interventional Pain Management
- Interventional Spine
- Intraarticular Calcaneal Fracture
- Joint Replacement
- Knee & Leg
- Kyphoplasty (Balloon Vertebroplasty)
- Kyphosis
- Labral Tears Of The Hip (Acetabular Labrum Tears)
- Laminectomy: Decompression Surgery
- Lateral Collateral Ligament (LCL) Injuries
- Lisfranc Injuries
- Little League Shoulder
- LITTLE LEAGUER'S ELBOW (MEDIAL APOPHYSITIS)
- Lumbar Epidural Steroid Injection
- Lumbar Interbody Fusion (IBF)
- MACI
- Mallet, Hammer & Claw Toes
- Medial Collateral Ligament Injuries
- Meniscus Tears
- Metatarsalgia
- Minimally Invasive Spine Surgery
- Morton’s Neuroma
- Muscle Spasms
- Muscle Strains of The Calf
- Nerve Pain
- Neuromas (Foot)
- Neurosurgery
- Olecranon Stress Fractures
- Orthopaedic Total Wellness
- Orthopaedic Trauma
- Orthopedic Physician Or A Podiatrist? Definition of a Podiatrist
- Osteoarthritis of the Hip
- Osteoporosis
- Outpatient Spine Surgery
- Partial Knee Replacement
- Patellar Fracture
- Pelvic Ring Fractures
- Peripheral Nerve Surgery (Hand) Revision
- Pinched Nerve
- Piriformis Syndrome
- Piriformis Syndrome
- Plantar Fasciitis
- Plastic Surgery
- Podiatry
- Primary Care Sports Medicine
- Quadriceps Tendon Tear
- Radial Tunnel Syndrome (Entrapment of the Radial Nerve)
- Revascularization of the Hand
- Reverse Total Shoulder Replacement
- Rheumatoid Arthritis (RA) of the Shoulder
- Rheumatoid Arthritis Of The Hand
- Robotics
- Rotator Cuff Tears
- Runner's Knee
- Sacroiliac Joint Pain
- Sciatica
- Scoliosis
- Senior Strong
- Shin Splints
- Shoulder
- Shoulder Arthritis
- Shoulder Arthroscopy
- Shoulder Injury: Pain In The Overhead Athlete
- Shoulder Replacement
- Shoulder Separations
- Shoulder Socket Fracture (Glenoid Fracture)
- SLAP Tears & Repairs
- Spinal Fusion
- Spine
- Spondylolisthesis and Spondylolysis
- Sports Foot Injuries
- Sports Hernias (Athletic Pubalgia)
- Sports Medicine
- Sports Wrist and Hand Injuries
- Sprained Ankle
- Sprained Wrist Symptoms and Treatment
- Subacromial Decompression
- Sudden (Acute) Finger, Hand & Wrist Injuries
- Targeted Muscle Reinnervation (TMR)
- Tendon Transfers of The Hand
- Tennis Elbow Treatment
- Thigh Fractures
- Thigh Muscle Strains
- Thumb Ulnar Collateral Ligament Injuries
- Total Ankle Replacement
- Total Hip Arthroplasty
- Total Hip Replacement - Anterior Approach
- Total Knee Replacement Surgery
- Trapezius Strain (Muscle Strain of The Upper Back)
- Traumatic Shoulder Instability
- Tricep Pain & Tendonitis
- Trigger Finger
- Turf Toe
- UCL (Ulnar Collateral Ligament) Injuries
- Ulnar Neuritis
- Valgus Extension Overload
- Vertebroplasty
- WALANT (Wide Awake Local Anesthesia No Tourniquet)
- Whiplash and Whiplash Associated Disorder (WAD)
- Wound Care
- Wrist Arthroscopy
- Wrist Fractures
- Wrist Tendonitis
Services
- Physical Medicine & Rehabilitation
- Physical Therapy
- Primary Care Sports Medicine
- PROMs (Patient-Reported Outcome Measures)
- Same-Day Orthopaedic Appointments Now Available
- Sports Medicine
- Sports-Related Concussion Treatment
- Telehealth Page
- Telemedicine
- Workers' Compensation
- Workers' Compensation Dispensary
- X-Ray
