Opioid Alternative Treatments
Millions of Americans suffer from chronic headaches or back pain. Others are recovering from surgery, sports injuries, or accidents. Every year, prescription opioids are used to treat moderate-to-severe pain. Because they have several serious side effects, it is important to learn more about the benefits and risks of opioids. Prescription opioids are powerful, can cause serious side effects, and lead to addiction.
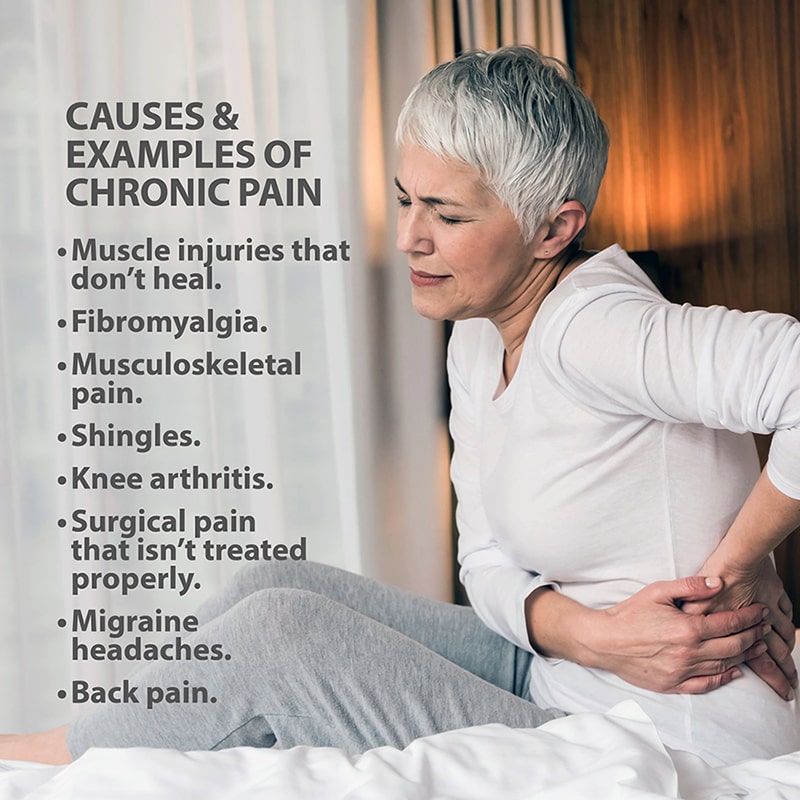
CHRONIC PAIN
More than 100 million American adults suffer from chronic pain. Chronic pain is pain that doesn’t go away and lasts three months or longer. Common causes include muscle injuries that don’t heal, fibromyalgia, musculoskeletal pain, and shingles.
Examples of chronic pain include:
- Arthritis in your knees.
- Surgical pain that isn’t treated properly.
- Migraine headaches.
- Back pain.
When pain lasts fewer than three months, it is considered acute pain. It can be pain that starts suddenly in response to an injury like a cut, bruise, burn, a broken bone, or pulled muscle. Acute pain also occurs after surgery. It can be caused by a fever, infection, or labor contractions. Labor pain, postoperative pain, and broken bones are all examples of acute pain, which can be effectively managed for most people with medication, physical therapy, and massage.
Sometimes acute pain can become chronic pain. A sports injury that isn’t diagnosed and treated correctly can lead to long-term damage to joints or muscles. Certain injuries can cause nerve damage. Postoperative pain that isn’t managed appropriately can lead to chronic pain.
OPIOIDS
Opioids (narcotics) are medications prescribed by physicians to treat persistent, acute, or severe pain. They can be part of effective pain management for people recovering from surgery or experiencing severe pain associated with cancer, serious injuries (such as falls or auto accidents), or from severe, chronic conditions like migraine headaches or fibromyalgia. Opioids can lead to addiction and overdose. They can and should only be used under the careful supervision of a physician.
Besides addiction, opioids have serious side effects, including some that are life-threatening. Opioid side effects include sleepiness, constipation, nausea, shallow breathing, slowed heart rate, and loss of consciousness.
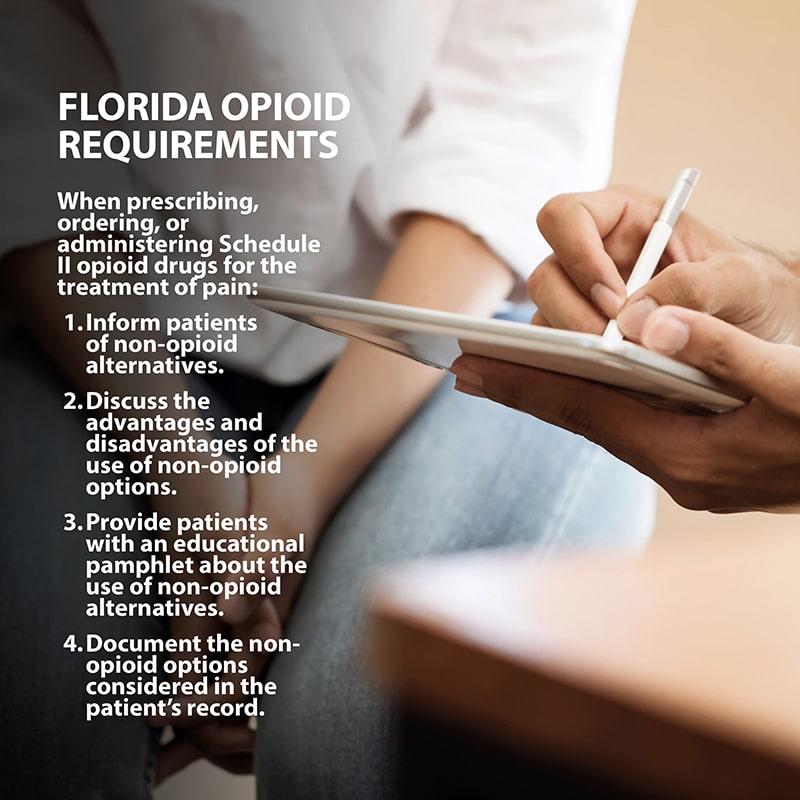
In Florida, health care practitioners are required to do the following when prescribing, ordering, or administering Schedule II opioid drugs for the treatment of pain:
- Inform patients of non-opioid alternatives for the treatment of pain.
- Discuss the advantages and disadvantages of the use of non-opioid options, including whether the patients are at high risk of or has a history of controlled substance abuse or misuse and the patient’s personal preferences.
- Provide patients with an educational pamphlet about the use of non-opioid alternatives created by the Florida Department of Health.
- Document the non-opioid options considered in the patient’s record.
OPIOID-ALTERNATIVE MEDICATIONS
There are many over-the-counter opioid-alternative medication options, such as Tylenol (acetaminophen) and aspirin, Motrin, and Advil (non-steroidal anti-inflammatory drugs-NSAIDs). Your physician may recommend using Advil/Motrin (ibuprofen) in combination with Tylenol (acetaminophen) depending on the type and cause of your pain. This combination can be as effective as opioids in controlling pain. These medications should only be combined as directed by a physician.
Your physician may also prescribe antidepressants, anti-seizure medications or steroids and suggest a combination of medications to address different aspects of your pain.
OTHER ALTERNATIVES
Medication may not be the only effective option for relieving your pain. Relief can be found with non-drug therapies used alone or in combination with drugs. These non-drug therapies include physical therapy, acupuncture, surgery, injections, and nerve blocks. Many patients also find relief with high-tech treatments using radio waves and electrical signals. Massages and other relaxation techniques, including biofeedback, where you learn to control involuntary functions such as heart rate, can bring pain relief.
ACUPUNCTURE – You may find relief from acupuncture, where thin needles are inserted at different places in your skin to interrupt pain signals.
CHIROPRACTIC CARE – Using manual, mechanical, electrical, natural methods, physical therapy, nutrition and acupuncture, chiropractic physicians treat and rehabilitate pain, diseases, and conditions. Chiropractors use a hands-on, prescription drug-free approach to health care to treat neuromusculoskeletal complaints, including back pain, neck pain, pain in the joints of the arms or legs, and headaches.
ELECTRICAL SIGNALS – Transcutaneous electrical nerve stimulation can provide short-term pain relief, especially for various types of muscle pain. This technique sends low-voltage electrical signals from a small device to the painful area through pads attached to the skin. While researchers aren’t exactly sure why it works, they think it may either interrupt the nerve signals to the brain or stimulate the production of “feel good” endorphins – the body’s natural painkillers.
INJECTIONS OR NERVE BLOCKS – If you have muscle spasms or nerve pain, injections with local anesthetics or other medications can help short-circuit the pain.
NERVE BLOCKS – Using X-ray imaging, pain medicine physicians can inject numbing medication that blocks or dampens pain and might even stop chronic pain from developing. The location of the injection depends on the source and type of pain. For example, pain in the arm or face can be relieved by blocking nerves in the neck. Relief may need a series of injections and repeated treatment.
PAIN PUMPS – Special pumps can be implanted to allow a patient to push a button and deliver pain medications to their spinal cord. This can bring relief without the side effects that often come with taking these drugs by mouth. Patients also get a psychological boost by having direct control over their pain. These spinal drug pumps are used most often by people with cancer pain and by patients with other types of pain who had side effects when orally taking the medication.
PHYSICAL THERAPY – A physical therapist or physician who specializes in physical medicine and rehabilitation can create an exercise program that helps improve your ability to function and decreases your pain. Whirlpools, ultrasound, and deep-muscle massages may also help.
RADIO WAVES – Radiofrequency ablation involves inserting a needle next to the nerve responsible for the pain. The electric current created by radio waves burns the nerve, short-circuiting the pain signal.
SPINAL CORD STIMULATION – When other methods fail, your physician might recommend spinal cord stimulation (SCS), which uses a pacemaker-like device that replaces the pain with a more tolerable sensation (typically a tingling or massage-like feeling.) The device is implanted in the lower back, attached to tiny wires that are in the spinal canal. When patients feel pain, they can use a remote control to send signals to the painful area. This technique can help with back pain as well as nerve damage in the legs that causes numbness and pain (neuropathy), common in people with diabetes. New forms of SCS show promise in relieving pain without the tingling.
SURGERY – When other treatments aren’t effective, surgery can be performed to correct abnormalities in your body that may be responsible for your pain.
If you suffer from chronic pain and would like to discuss non-opioid alternative treatments, contact the specially trained physicians at Florida Orthopaedic Institute.
DOWNLOAD THIS PAMPHLET ON NONOPIOID ALTERNATIVES
The following Florida Orthopaedic Institute physicians specialize in Opioid Alternative Treatments:
Specialties
- AC Joint Injuries
- Achilles Tendinitis - Achilles Insertional Calcific Tendinopathy (ACIT)
- Achilles Tendon Rupture
- Achilles Tendonitis
- ACL Injuries
- Ankle Fracture Surgery
- Ankle Fractures (Broken Ankle)
- Ankle Fusion Surgery
- Anterior Cervical Corpectomy & Discectomy
- Arthroscopic Articular Cartilage Repair
- Arthroscopic Chondroplasty
- Arthroscopic Debridement of the Elbow
- Arthroscopy Of the Ankle
- Articular Cartilage Restoration
- Artificial Disk Replacement (ADR)
- Aspiration of the Olecranon Bursa - Fluid In Elbow
- Atraumatic Shoulder Instability
- Avascular Necrosis (Osteonecrosis)
- Bankart Repair
- Basal Joint Surgery
- Bicep Tendon Tear
- Bicep Tenodesis
- Bone Cement Injection
- Bone Growth Stimulation
- Bone Health Clinic
- Broken Collarbone
- Bunions
- Bursitis of the Shoulder (Subacromial Bursitis)
- Calcific Tendinitis of the Shoulder
- Carpal Tunnel Syndrome
- Charcot Joint
- Chiropractic
- Clavicle Fractures
- Colles’ Fractures (Broken Wrist)
- Common Foot Fractures in Athletes
- Community Outreach
- Cubital Tunnel Syndrome
- De Quervain's Tenosynovitis
- Deep Thigh Bruising
- Degenerative Disk Disease
- Diffuse Idiopathic Skeletal Hyperostosis (DISH)
- Discectomy
- Discitis Treatment & Information
- Dislocated Shoulder
- Dupuytren’s Disease
- Elbow
- Elbow Bursitis
- Elbow Injuries & Inner Elbow Pain in Throwing Athletes
- Epidural Injections for Spinal Pain
- Finger Dislocation
- Flexor Tendonitis
- Foot Stress Fractures
- Foot, Ankle & Lower Leg
- Foraminotomy
- Fractured Fingers
- Fractures Of The Shoulder Blade (Scapula)
- Fractures Of The Tibial Spine
- Functional Nerve Transfers of The Hand
- Ganglion Cysts
- General Orthopedics
- Glenoid Labrum Tear
- Golfer's Elbow
- Groin Strains and Pulls
- Growth Plate Injuries Of The Elbow
- Hallux Rigidus Surgery - Cheilectomy
- Hammer Toe
- Hamstring Injuries
- Hand & Finger Replantation
- Hand & Wrist
- Hand Nerve Decompression
- Hand Skin Grafts
- Hand, Wrist, Elbow & Shoulder
- Heat Injury/Heat Prostration
- High Ankle Sprain (Syndesmosis Ligament Injury)
- Hip & Thigh
- Hip Arthroscopy
- Hip Dislocation
- Hip Flexor Strains
- Hip Fractures
- Hip Hemiarthroplasty
- Hip Impingement Labral Tears
- Hip Muscle Strains
- Hip Pointers and Trochanteric Bursitis
- Hyperextension Injury of the Elbow
- Iliopsoas Tenotomy
- Iliotibial Band Syndrome
- Impingement Syndrome of the Shoulder
- Interlaminar Implants
- Interlaminar Lumbar Instrumental Fusion: ILIF
- Interventional Pain Management
- Interventional Spine
- Intraarticular Calcaneal Fracture
- Joint Replacement
- Knee & Leg
- Kyphoplasty (Balloon Vertebroplasty)
- Kyphosis
- Labral Tears Of The Hip (Acetabular Labrum Tears)
- Laminectomy: Decompression Surgery
- Lateral Collateral Ligament (LCL) Injuries
- Lisfranc Injuries
- Little League Shoulder
- LITTLE LEAGUER'S ELBOW (MEDIAL APOPHYSITIS)
- Lumbar Epidural Steroid Injection
- Lumbar Interbody Fusion (IBF)
- MACI
- Mallet, Hammer & Claw Toes
- Medial Collateral Ligament Injuries
- Meniscus Tears
- Metatarsalgia
- Minimally Invasive Spine Surgery
- Morton’s Neuroma
- Muscle Spasms
- Muscle Strains of The Calf
- Nerve Pain
- Neuromas (Foot)
- Neurosurgery
- Olecranon Stress Fractures
- Orthopaedic Total Wellness
- Orthopaedic Trauma
- Orthopedic Physician Or A Podiatrist? Definition of a Podiatrist
- Osteoarthritis of the Hip
- Osteoporosis
- Outpatient Spine Surgery
- Partial Knee Replacement
- Patellar Fracture
- Pelvic Ring Fractures
- Peripheral Nerve Surgery (Hand) Revision
- Pinched Nerve
- Piriformis Syndrome
- Piriformis Syndrome
- Plantar Fasciitis
- Plastic Surgery
- Podiatry
- Primary Care Sports Medicine
- Quadriceps Tendon Tear
- Radial Tunnel Syndrome (Entrapment of the Radial Nerve)
- Revascularization of the Hand
- Reverse Total Shoulder Replacement
- Rheumatoid Arthritis (RA) of the Shoulder
- Rheumatoid Arthritis Of The Hand
- Robotics
- Rotator Cuff Tears
- Runner's Knee
- Sacroiliac Joint Pain
- Sciatica
- Scoliosis
- Senior Strong
- Shin Splints
- Shoulder
- Shoulder Arthritis
- Shoulder Arthroscopy
- Shoulder Injury: Pain In The Overhead Athlete
- Shoulder Replacement
- Shoulder Separations
- Shoulder Socket Fracture (Glenoid Fracture)
- SLAP Tears & Repairs
- Spinal Fusion
- Spine
- Spondylolisthesis and Spondylolysis
- Sports Foot Injuries
- Sports Hernias (Athletic Pubalgia)
- Sports Medicine
- Sports Wrist and Hand Injuries
- Sprained Ankle
- Sprained Wrist Symptoms and Treatment
- Subacromial Decompression
- Sudden (Acute) Finger, Hand & Wrist Injuries
- Targeted Muscle Reinnervation (TMR)
- Tendon Transfers of The Hand
- Tennis Elbow Treatment
- Thigh Fractures
- Thigh Muscle Strains
- Thumb Ulnar Collateral Ligament Injuries
- Total Ankle Replacement
- Total Hip Arthroplasty
- Total Hip Replacement - Anterior Approach
- Total Knee Replacement Surgery
- Trapezius Strain (Muscle Strain of The Upper Back)
- Traumatic Shoulder Instability
- Tricep Pain & Tendonitis
- Trigger Finger
- Turf Toe
- UCL (Ulnar Collateral Ligament) Injuries
- Ulnar Neuritis
- Valgus Extension Overload
- Vertebroplasty
- WALANT (Wide Awake Local Anesthesia No Tourniquet)
- Whiplash and Whiplash Associated Disorder (WAD)
- Wound Care
- Wrist Arthroscopy
- Wrist Fractures
- Wrist Tendonitis
Services
- Physical Medicine & Rehabilitation
- Physical Therapy
- Primary Care Sports Medicine
- PROMs (Patient-Reported Outcome Measures)
- Same-Day Orthopaedic Appointments Now Available
- Sports Medicine
- Sports-Related Concussion Treatment
- Telehealth Page
- Telemedicine
- Workers' Compensation
- Workers' Compensation Dispensary
- X-Ray
