Discitis treatment & information
Discitis is an infection that happens between the vertebrae of your spine. It is a complicated infection to treat since the vertebrae have low blood supply, and most antibiotics are transmitted through the bloodstream. There are no surgical procedures available to treat this particular infection, but there are special IV antibiotic treatments as well as other nonsurgical treatments available to get you back on your feet.
Anatomy
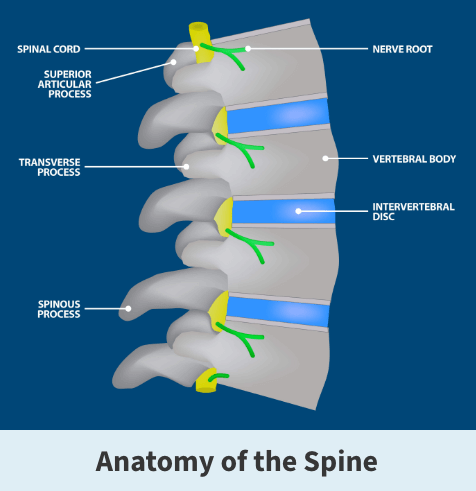
The spine consists of 33 individual bones (vertebrae) that interlock. The vertebrae are categorized into five regions:
- Cervical
- Thoracic
- Lumbar
- Sacrum
- Coccyx
Intervertebral discs sit between the vertebrae and are the shock absorbers for the spine. They are flat, round, about half an inch thick and made up of two components — the nucleus pulposus and the annulus fibrosus. The nucleus has a jelly-like consistency, found in the center of the disc. The “jelly” allows the disc to be flexible and strong. The annulus is the flexible outer ring of the disc and consists of several layers. When moving or standing, weight is put on the nucleus, causing it to expand while the annulus holds it in place. Together, the nucleus and annulus allow for movement to take place while simultaneously maintaining the strength of the spine.
About
Discitis is a rare infection of the discs between the vertebra of the spine and is very difficult to treat. Like appendicitis, this illness is usually a bacterial infection, but can also be viral. Spinal discs do not have a strong blood supply, so if the bacteria or virus are there, it is tough for the body’s immune cells to reach and heal the infection. Another issue is that since medication used to heal infections (like antibiotics) travels through the bloodstream, spinal infections cannot easily be treated with antibiotics because the medication may never make it to the infection.
There are two types of discitis. One is the result of interference at the site of the infection by a surgical, diagnostic, or therapeutic procedure. For example, surgery on the back or a needle placed in the back can introduce pathogens, a bacterium, virus, or other microorganisms that can cause disease.
The other type is “spontaneous” discitis, caused by an infecting organism, either bacterial or viral, that comes to the disc by the blood from the kidney, bladder, nose, throat, lungs, intestine, gums, pelvic infections, or any other entry into the body. This usually causes a blood-borne attack that leads to an infection.
Symptoms
If you have discitis, you will probably experience severe pain in part of your spine.
Other symptoms can include:
- Changes in your posture
- Stiffness in your back
- Difficulty performing regular mobility tasks
- Abdominal pain or discomfort
- Fever

Diagnosis
Your Florida Orthopaedic Institute physician will take a look at your symptoms and choose to order some tests to get a better idea of your symptoms. These tests may include:
- Blood tests – This test collects a sample of your blood which gives a red and white blood cells count which can help diagnose infection.
- Bone scans – This test is used to take a more in-depth look at your vertebrae, which can help your physician assess the vitality of the bone and learn if you have a bone infection.
- Imaging tests – These tests create pictures of your spine as well as the surrounding tissues. Some examples of these types of tests include X-rays and MRIs.
- Tissue analysis – In some cases, your physician may order a biopsy of your spinal tissue to collect a sample for analysis. This can help them develop their diagnosis.
Treatment
Although this type of spinal infection is difficult to treat, it is treatable and usually results in an uncomplicated cure. That being said, it takes a very long course of antibiotic therapy given intravenously (through an IV), every day at an infusion center. The standard treatment requires six to eight weeks of this antibiotic therapy. Pain is treated with painkillers and patients should move as little as possible, and a brace may be recommended to enforce this.
Activity of other parts of the body not affected, like arm exercises, should be done to prevent generalized weakness. Eating a healthy diet and responsible drinking are probably important. The prolonged treatment course and the considerable pain and immobility can lead to situational depression that is treated if present.
Related specialties
- Anterior Cervical Corpectomy & Discectomy
- Artificial Disc Replacement (ADR)
- Bone Cement Injection
- Degenerative Disc Disease
- Diffuse Idiopathic Skeletal Hyperostosis (DISH)
- Discectomy
- Epidural Injections for Spinal Pain
- Foraminotomy
- Interlaminar Implants
- Interlaminar Lumbar Instrumental Fusion: ILIF
- Kyphoplasty (Balloon Vertebroplasty)
- Kyphosis
- Laminectomy: Decompression Surgery
- Lumbar Epidural Steroid Injection
- Lumbar Interbody Fusion (IBF)
- Minimally Invasive Spine Surgery
- Outpatient Spine Surgery
- Pinched Nerve
- Piriformis Syndrome
- Sacroiliac Joint Pain
- Sciatica
- Scoliosis
- Spinal Fusion
- Spondylolisthesis & Spondylolysis
- Vertebroplasty
- Whiplash & Whiplash Associated Disorder (WAD)
