Learn everything you need to know about sudden acute finger, hand and wrist injuries in our comprehensive guide.
Sudden acute finger, hand & wrist injuries
Though often overlooked, your hands, fingers, and wrists play a critical role in your life. Few, if any, activities can be performed without them. When they sustain an injury, an individual’s lifestyle, and ability to perform many basic tasks are often challenged.
Sudden injuries to the hands, fingers, and wrists are relatively common. Even though most of our movements don’t cause problems, symptoms can develop from everyday wear and tear, injuries, or overuse. Often these events are mild and heal on their own. More severe ones can need surgery.
Anatomy
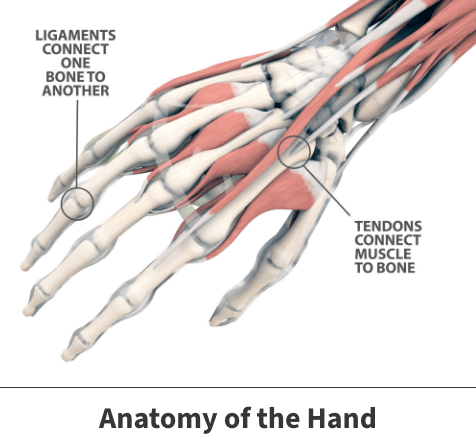
The hand and wrist consist of dozens of bones, joints, ligaments, tendons, and muscles that need to work together seamlessly in a variety of positions hundreds of times a day. As such, they often require highly specialized medical care when they become injured.
About
The most common finger, hand, and wrist injuries happen during or from:
- Sports
- Recreational activities
- At work
- Projects around the home (especially when using machinery)
- Fights
- Falls
- Soft tissue inflammation
- Work-related stress
- Participation in home improvement projects
Wrestling, football, soccer, and other contact sports have a higher risk of finger, hand, or wrist injury. The same is true for higher-speed sports, such as biking, in-line skating, skiing, snowboarding, and skateboarding. Other sports that bear weight on the hands and arms (such as gymnastics) increase the risk of injury. There is also an increased risk of injury for sports that use hand equipment such as ski poles, hockey or lacrosse sticks, or racquets.
Individuals also at higher risk include those employed in professions requiring continual, awkward, or forceful hand motions, older persons with decreasing bone and muscle mass levels, those with underlying inflammation-causing illnesses, and persons with balance or vision problems.
Most children’s finger, hand, or wrist injuries occur during sports, play, or accidental falls. In children, injuries at the end of a long bone near a joint may damage the growth plate (physis) and should always be examined by a doctor.
We lose muscle mass and bone strength (osteopenia) when we age, putting older adults at higher risk for injuries and fractures. Balance and vision problems also increase the risk of accidental injury.

Sudden (acute) injuries
Sudden (medically known as acute) injuries can occur following direct blows, falls, or any motion in which a hand, finger, or wrist is unusually bent, twisted, or jerked. Acute problems are often caused by accidents like falls or automobile collisions. Acute injuries include the following:
Bruises
Bruises usually occur after skin and bones receive some type of forceful contact. These occurrences often result in pain and discoloration of affected skin. In most cases, bruises heal on their own.
Sprains
Sprains happen when soft tissues, known as ligaments, are hurt. Ligaments connect bones together. Sprains are sometimes mistaken for broken bones because the injury can cause both a sprain and a fracture in the same area. Symptoms can be mild or severe and are classified as first-degree, second-degree, and third-degree sprains.
First-degree sprains are when the ligament is stretched but not torn. There is usually mild to moderate pain and swelling. The joint is stable and is not loose or wobbly. The joint moves normally but is typically painful.
Second-degree sprains partially tear the ligament. A pop or snap may be felt or heard at the time of the injury. Moderate to severe pain and swelling restricts movement. The joint may be mild to moderately unstable and look bruised.
Third-degree sprains completely tear the ligament with a pop or snap at the time of the injury. Sometimes less than with a partial tear, symptoms include mild to severe pain, swelling, and bruising. Joints can feel loose or wobbly with a grating sound when trying to move them. A bulge is typical at the site of a complete tear, along with numbness or tingling.
Symptoms vary depending on how bad the ligament damage is. Most sprains will involve at least some level of pain and swelling. Moderate to severe injuries might also cause instability and movement issues making even the smallest everyday tasks challenging.
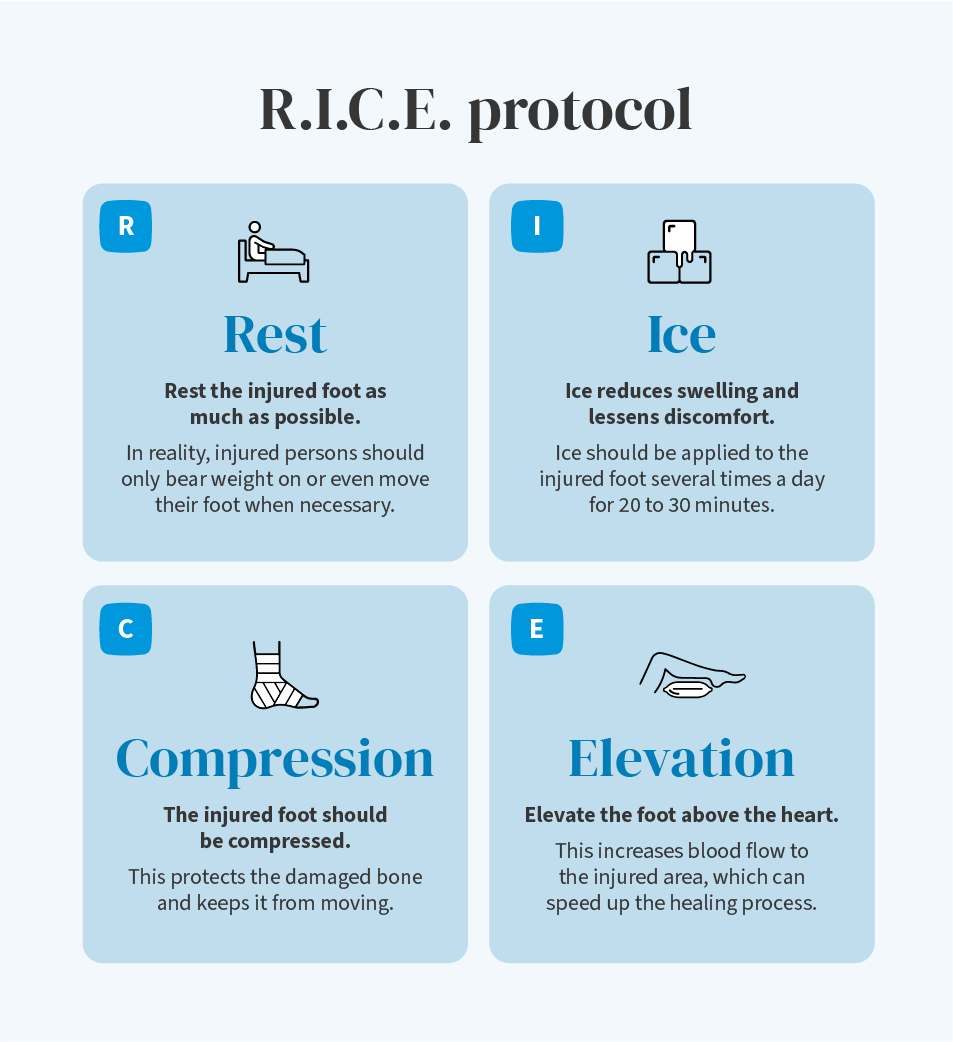
Treatment will depend on severity. Mild to moderate occurrences often heal with time and a method abbreviated as RICE. An easy way to remember this treatment is to use the acronym RICE: Rest, Ice, Compression, and Elevation. This treatment should be used as soon as possible after a sprain to relieve pain and swelling and promote healing and flexibility.
- Rest – Rest and protect the sore or injured area. Take a break, change, or stop any activity causing the pain or soreness.
- Ice – Cold reduces pain and swelling. Apply ice or a cold pack immediately to prevent and reduce swelling. Apply it for 10 to 20 minutes – three or more times a day. You can apply heat to the area if the swelling is gone after 48 to 72 hours. Never apply ice or heat directly to the skin – place a towel between the cold or heat pack and the skin.
- Compression – Wrapping the injured or sore area with an elastic bandage (such as an Ace bandage) helps decrease swelling. Don’t wrap too tightly, as this can cause swelling below the affected area. Check the wrap and look for signs that the bandage is too tight (numbness, tingling, increased pain, coolness, or swelling) in the area below the bandage. If the bandage gets too tight, loosen it. If you need to use compression for longer than 48 to 72 hours, contact your doctor to ensure there’s not a more serious problem.
- Elevation – Anytime you sit or lie down, raise the injured area with pillows while applying ice. If you can keep the area at or above the level of your heart, it will help reduce swelling.
Advil or Motrin (ibuprofen) and Aleve or Naprosyn (naproxen) are nonsteroidal over-the-counter anti-inflammatories that help relieve pain and swelling.
Minor sprains often heal well with home treatment, but in more serious cases, your doctor might place the injured hand into a movement-restricting device like a cast or splint. Moderate to severe sprains might also need a course of physical therapy, pain-relieving medications, or possibly even surgery to repair and reconnect the damaged tissues.
Recovery times for sprains vary depending on a person’s age and health and the location and severity of the injury.
Skier’s thumb
This injury impacts the thumb ligament (the ulnar collateral ligament – abbreviated the UCL). This injury is most often seen in skiers who experience falls holding their poles. Injuries can involve stretching and partial or complete tears. Treatment will be given based on the injury’s severity. Skier’s Thumb is also called Gamekeeper’s Thumb.
Injuries to tendons (mallet finger)
Mallet finger (also known as baseball finger or drop finger) impacts finger tendons. Tendons are the soft tissues joining muscles and bones. This event typically occurs in baseball players and happens when one tries to catch a ball, and their fingertip is hit with significant force. Often, this results in tendon rupture, causing pain and swelling.
Splints straighten the injured finger in anywhere from four to six weeks. Severe occurrences might need surgery.
Strains (pulled muscles)
Overstretching muscles causes most strains. They can be severe, such as a torn muscle or tendon, or minor. Symptoms of a strain vary depending on the severity of the strain and can include:
- Pain
- Tenderness (that is worse with movement)
- Swelling
- Bruising
- Limited muscle movement
- A bulge at the site of a complete tear
While minor strains often heal well with home treatment, severe strains need medical treatment. Severe injuries may need surgery to repair damaged muscles. Additionally, like sprains, serious strains could eventually lead to long-term pain, limited movement, deformity, and permanent damage.
Broken bones (fractures)
Fractures are breaks in a bone that can range from hairline cracks to bones broken into two or more pieces. Fractures can occur at the same time as other injuries, such as sprains, strains, or dislocations.
Symptoms of bone fractures include:
- Pain
- Pain that worsens when the broken bone is moved
- Swelling
- Bruising
- Popping or snapping sounds when the injury occurs
- Limited movement
- Bone movement where there is no joint (for example, a bend in the arm between the elbow and wrist)
- Bone poking through the skin
- Bone visible in the wound
The broken bone might push through the surrounding skin in the most severe cases, known as open fractures.
Fractures need medical evaluation and treatment. Usually, broken bones are placed into movement-restricting devices (casts or splints) to promote healing and prevent further injury. Some fractures may need surgery. This is especially true of complicated events like open breaks that can increase the chance of infection.
Recovery times vary depending on many factors. They can range from weeks to months, depending on age, health, type of fracture, and the location and severity of the fracture. Other injuries may complicate treatment.
Dislocations
Dislocations are when a bone is pulled or pushed out of place and out of its normal relationship to the other bones that make up a joint. They are caused by direct blows to a joint, falls, or sudden twisting movements. Even everyday activities can cause dislocations if a person has unstable joints.
Treatment is usually focused on repositioning the misplaced bone. Often, placing the dislocated finger into a splint or cast will promote healing within several weeks. The most severe events may need to be repositioned surgically.
Dislocations can be problems even if the bone pops back into place. Soft tissues in or around a joint (such as ligaments, tendons, muscles, cartilage, and the joint capsule) can stretch or tear. Nerves and blood vessels can be damaged. Pieces of bone at the base of the joint can break off and end up inside the joint. Dislocations can cause fractures that extend into the joint.
Compartment syndrome from a crushing injury
Compartment syndrome develops when swelling occurs within an enclosed area (a compartment) in which muscles, nerves, blood vessels, and bones have no room to expand. Pressure on arteries, veins, and nerves causes extreme pain, slows circulation to the muscles and nerves, and can cause permanent damage to the tissue.
Swelling that causes compartment syndrome is usually caused by decreased blood flow, trauma, bleeding, and fluid buildup. Compartment syndrome requires immediate emergency medical treatment to prevent tissue death and permanent dysfunction.
People involved in a significantly increased level of physical activity, such as long-distance runners or new military recruits, can develop chronic compartment syndrome.
Treatment
Treatment for any sudden acute finger, hand, or wrist injury will hinge on several underlying considerations such as their severity, location, if other injuries are present, and the individual’s age, health, and fitness level.
Most simple, uncomplicated finger, hand, and wrist injuries heal with conservative treatments such as rest, the application of ice, and the occasional use of pain and inflammation-reducing medications.
Moderate injuries might also need a course of physical therapy to help the injured person regain any strength or motion their finger, hand, or wrist lost.
Severe issues may need surgery. This is especially true of serious sprains and bone fractures, which could increase the risk of complications like infection or damage to other vital physical features like blood vessels and nerves.
Recovery
Mild injuries can heal within days or weeks. More severe wounds could take weeks or even months to improve fully. Doctors often hesitate to offer specific recovery times because many underlying factors influence the healing process.
Prevention
Preventing all hand, finger, and wrist injuries is impossible. You can lessen your risk by practicing preventative measures such as:
- Exercising bones and soft tissues
- Wearing protective coverings like gloves when using tools or heavy machinery
- Consuming a healthy diet filled with bone and tissue-strengthening nutrients
- Avoiding or limiting vices like cigarette smoking or excessive alcohol intake
Above all, individuals should schedule routine medical checkups where doctors can diagnose emerging physical injuries or treat inflammation-causing diseases.
Important considerations
Anyone with a finger, hand, or wrist injury should immediately seek medical attention. Time is of the essence as the potential for permanent damage. Destructive injury increases significantly when medical attention is delayed. Cuts and hand injuries need advanced treatment to prevent infection or loss of function, regardless of size.
Injuries to the hand with the following symptoms generally need emergency medical attention:
- Severe bleeding
- Numbness
- Loss of motion or strength
- Severe pain
- Obvious deformity
- Signs of infection (tenderness, local warmth, redness, swelling, pus, or fever)
- Exposure of underlying structures (tendons, bones, joints, arteries, veins, or nerves)
Certain injuries should prompt immediate medical attention, such as those with severe bleeding, numbness, visible deformities, signs of infection, deep cuts, and burns.
If you experience an unexpected bone, joint, or muscle injury, you can visit the only urgent care center in Tampa Bay specializing in orthopedics. We are open during regular business and extended hours Monday through Saturday at our South Tampa and Brandon locations. You get immediate orthopedic care for broken bones, strains and sprains, sports injuries, foot or ankle injuries, shoulder injuries, knee injuries, hand or wrist injuries, and back pain.
Florida Orthopaedic Institute’s Orthopaedic Urgent Care is a quicker and less expensive alternative to the hospital emergency room. Walk-ins are welcome, and you can call ahead to pre-register. Come to Florida Orthopedic Institute’s Urgent Care for faster service and lower cost than an emergency room. No appointment is necessary, and all ages are welcome.
Related specialties
- Basal Joint Surgery
- Carpal Tunnel Syndrome
- De Quervain's Tenosynovitis
- Dislocated Finger
- Distal Radius Fracture (Broken Wrist)
- Dupuytren’s Disease
- Flexor Tendonitis
- Fractured Fingers
- Functional Nerve Transfers of the Hand
- Ganglion Cysts
- Hand & Finger Replantation
- Hand Nerve Decompression
- Hand Skin Grafts
- Nerve Pain
- Peripheral Nerve Surgery (Hand) Revision
- Revascularization of the Hand
- Rheumatoid Arthritis of the Hand
- Sports Wrist & Hand Injuries
- Sprained Wrist
- Targeted Muscle Reinnervation (TMR)
- Tendon Transfers of the Hand
- Thumb Ulnar Collateral Ligament Injuries
- Trigger Finger
- Ulnar Neuritis
- WALANT (Wide Awake Local Anesthesia No Tourniquet)
- Wrist Arthroscopy
- Wrist Fractures
- Wrist Tendonitis