Thigh muscle strains
Straining a muscle, whether from sports or daily activity, is common for people of all ages. When a muscle is stretched beyond its limit, a tear can occur that can range from mild to serious. When the thigh is integral to high-speed activities such as football, running, soccer, and basketball, thigh muscle strains can occur relatively easily.
A muscle strain (pulled muscle) happens when your muscle is overstretched or torn due to overuse, fatigue, or improper use. Strains are commonly confused with sprains. A sprain is the stretching or tearing of the tough bands of fibrous tissue (ligaments) that connect two bones in your joints. Strains and sprains share similar signs and symptoms but involve different parts of your body.
Anatomy
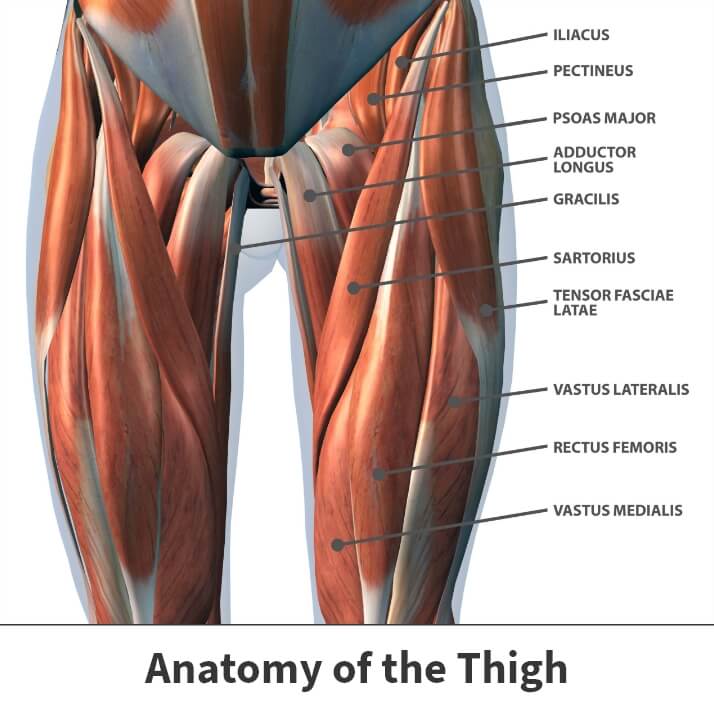
The thigh has three sets of muscles:
- Hamstring muscles – Located in the back of the thigh to extend and flex the leg.
- Quadriceps muscles – Located in the front of the thigh to extend and flex the leg.
- Adductor muscles – Located inside of the thigh to pull the legs together.
Since the hamstring and quadriceps muscles cross at the hip and knee, they are at a high risk of being strained. Also, muscles weaken when strained, so it is important to let them heal properly to avoid further damage.
About
Strains occur when muscle fibers are extended beyond their natural abilities and become torn. This tearing away of the muscle from the tendon can result in a painful injury if left unattended. An accident or injury that causes a direct blow to the thigh muscles can also create a serious strain. These injuries vary in severity. Mild strains involve only a slight overextension of muscle but no structural damage. Moderate strains happen when a part of the muscle tissue is torn. Severe injuries are those involving significant or complete muscle tears.
Causes
Thigh muscle strains usually result from some type of sudden or forceful movement. A significant percentage of cases occur during athletic activity. Events like falls might also produce such injuries. Other possible causes include poor muscle flexibility and pre-existing muscle tightness.
Risk factors
One’s risk of developing a thigh muscle strain increases in instances of:
- Muscle imbalance – Thigh muscles like the quadriceps and hamstrings work in tandem. In some people, one set of muscles is notably stronger than the other, leaving the weaker components more likely to sustain injury.
- Muscle fatigue – Overworked or tired muscles do not absorb enough energy to function correctly, leaving them weakened and susceptible to strains.
- Muscle weakness – Improperly exercised or weak muscles stand far more vulnerable to damage than appropriately worked and conditioned components.
- Inadequate workout preparation – Many strains result from failing to stretch the thigh muscles before engaging in physical activity or athletic competition.
Symptoms
Usually, those who experience a thigh muscle strain feel a snapping sensation in the thigh area. This sensation is the muscle tearing. This type of injury can create a more serious issue if the blood vessels are also broken. Additionally, a popping feeling can also be a sign of a pulled muscle in the thigh area, where the pain is severe and instant. The most obvious symptom is pain. This discomfort varies in intensity depending on the strain’s severity and location based on the specific muscles involved. In many instances, pain occurs suddenly and can be intense.
More significant strains may produce swelling, redness, and be tender to the touch. People might also experience visible bruising if surrounding blood vessels are damaged. Flexing or extending the damaged leg could prove difficult, resulting in mobility difficulties.
Diagnosis
When diagnosed, your Florida Orthopaedic Institute physician will discuss your history and any details about the injury. Then, they will ask you about your symptoms and examine the thigh for tenderness and bruising.
To determine mobility, your physician may ask you to bend and straighten your knee. In some instances, an x-ray or other diagnostics may take place to determine the severity of the injury. More specifically, muscle strains are graded based on their degree of severity, 1 being mild and 3 being severe. If it is a Grade 1 strain, it can heal relatively quickly, while a Grade 3 strain might take an extended time.
Treatment
After diagnosis, your physician will discuss all viable treatment options to determine the best choice for your injury. Since almost all thigh muscle strains can heal without surgery, your physician will likely recommend a combination of over-the-counter medicine and rest.
Nonsurgical treatments
If nonsurgical treatment is an option, the R.I.C.E. protocol is most commonly used to treat muscle strain injuries. This treatment can generally heal most thigh muscle strains without surgery.
R.I.C.E. stand for:
- Rest – Stop the activity you had been performing at the time of the injury while it heals.
- Ice – Use cold packs for 20 minutes several times a day. Do not apply ice directly to the skin.
- Compression – Wrap the injury in a soft compression bandage.
- Elevation – Raise your leg higher than your heart to minimize the swelling.
Besides R.I.C.E., your physician may recommend taking over-the-counter medicine to stop the pain and swelling. Non-steroidal anti-inflammatory medication (NSAIDs) such as ibuprofen (Motrin, Advil) can also assist with pain relief and healing.
As the injury heals, physical therapy can slowly create a better range of motion and build strength. These specially designed exercises help individuals strengthen wounded muscles and recapture motion lost during periods of inactivity.
Before returning to sports or regular physical activity, your thigh muscle should be completely healed. This is because full-strength, healthy muscles are the only kind that can combat future tears and additional injury.
What can you do to prevent a pulled muscle in the thigh?
While strain-causing events like falls cannot usually be prevented, there are various techniques you can use to prevent all muscle strains. Some common methods include:
- Dynamic stretching – active movements where joints and muscles go through a full range of motion.
- Efficiently warm up before strenuous activity – While exercise is important, it should never be rushed into. Many thigh muscle strains happen because people neglect to adequately stretch their muscles in preparation for the forceful movements to follow.
- Cross-training – weight lifting or resistance band training strengthens muscles outside the chosen sport or strenuous activity.
- Keeping muscles active – Exercise strengthens muscles. Engage in any type of leg-strengthening activity. Even walking several times per week stretches and extends thigh muscles.
- Eating foods with high potassium – such as bananas or avocados, can help prevent muscle fatigue.
- Staying properly hydrated – Water consumption is critical to muscle health. The failure to drink adequate amounts of water increases muscle cramping and fatigue.
- Observing necessary precautions – Once thigh pain develops, individuals should rest until the discomfort disappears or consult their doctor to determine the cause and begin any needed treatment.
Surgical treatments
If surgery is recommended, it will only be in the most severe cases. Most thigh muscle strains do not need surgical attention. Even Grade 3 strains can heal on their own through rest and physical therapy. During your initial diagnosis, your physician will determine the severity of the strain and discuss with you all treatment options available.
Recovery
Mild strains often heal within several weeks. Moderate strains might take a bit longer. Severe wounds might need several months before returning to full capacity. This is especially true if surgery is performed. Several considerations factor into one’s recovery timeframe, including their:
- General health
- Injury severity
- The treatment they underwent
- Fitness level before the injury
- Age
- Injury history
Other issues like diet, environment, and lifestyle habits might also increase or decrease recovery time.
Questions to ask your doctor about thigh muscle strains
- How do I know if I have a thigh muscle strain?
- What are the symptoms?
- Will I need an x-ray?
- How do you treat a thigh muscle strain?
- What are the risk factors?
- What precautions can I take to prevent future strains?
- Will I need physical therapy?
- What muscles are involved?
- How long will it take to heal?

Videos
Related specialties
- Anterior Hip Replacement
- Avascular Necrosis (Osteonecrosis)
- Groin Strains & Pulls
- Hamstring Injuries
- Hip Arthroplasty
- Hip Arthroscopy
- Hip Dislocation
- Hip Flexor Strains
- Hip Fractures
- Hip Hemiarthroplasty
- Hip Impingement Labral Tears
- Hip Muscle Strains
- Hip Pointers & Trochanteric Bursitis
- Iliopsoas Tenotomy
- Labral Tears of the Hip (Acetabular Labrum Tears)
- Osteoarthritis of the Hip
- Osteoporosis
- Pelvic Ring Fractures
- Piriformis Syndrome
- Sports Hernias (Athletic Pubalgia)
- Thigh Fractures
