Osteoarthritis of the Hip
OVERVIEW
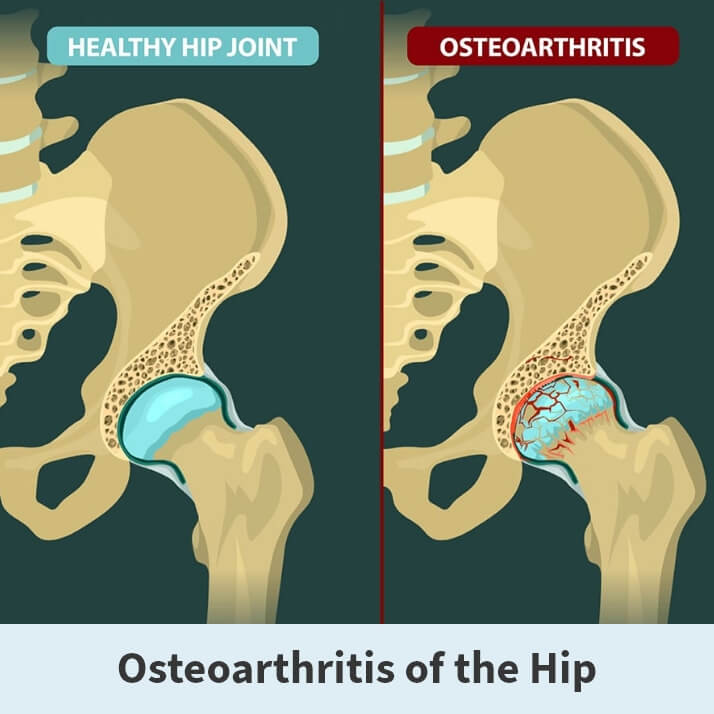
Osteoarthritis of the hip is a “wear-and-tear” disease. The cartilage of the hip joint gradually wears away over time, causing pain and stiffness. It can make it hard to do everyday activities like bending over to tie a shoe, rising from a chair, or taking a short walk.
Since osteoarthritis gradually worsens over time, the sooner you start treatment, the more likely it is that you can lessen its impact on your life. Unfortunately, there is no cure for osteoarthritis. But there are many nonsurgical and surgical treatment options available to help you manage pain, stay active, and live the best life you can.
ANATOMY
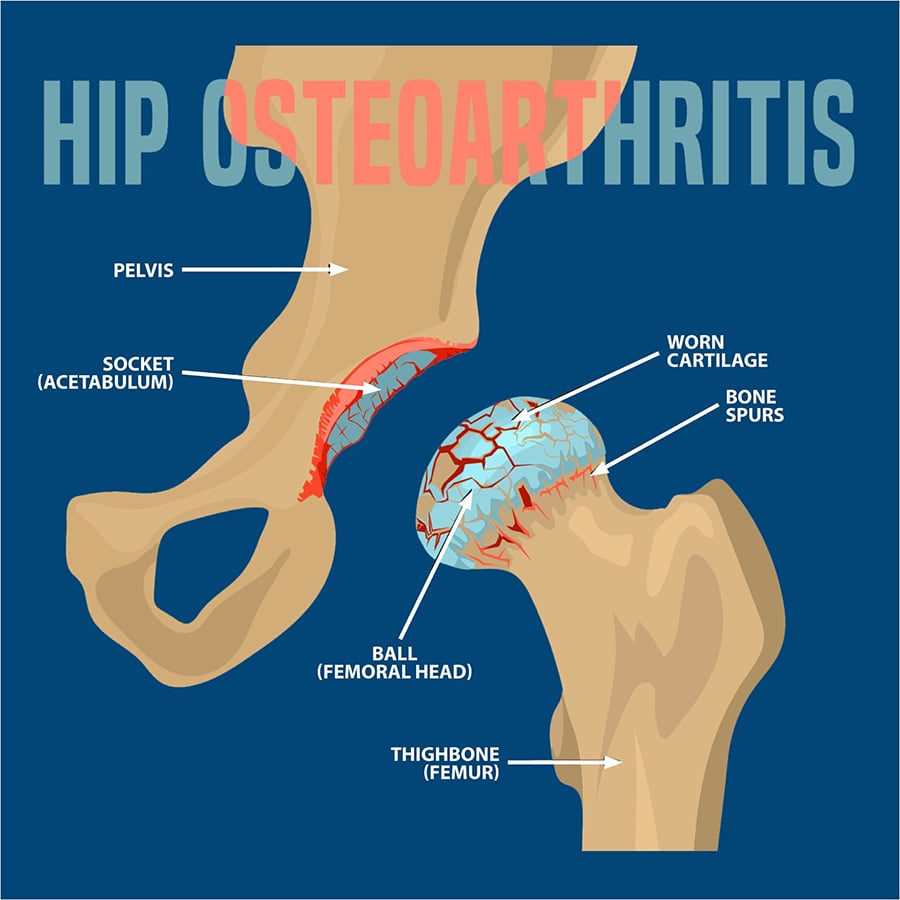
The hip is a ball and socket joint. The socket is formed by the large pelvic bone (acetabulum), and the ball is formed by the upper end of the thighbone (femoral head). A slippery tissue known as the articular cartilage covers the surface of the joint, creating a smooth surface that allows the bones to glide easily across each other. The large pelvic bone is ringed by strong fibrocartilage known as the labrum, which form a lining around the socket.
Also, the whole joint is surrounded by bands of tissue (ligaments) that form a capsule that acts to hold the joint together. The undersurface of the capsule is lined by a thin membrane (synovium), which produces synovial fluid to lubricate the hip joint.
DESCRIPTION
Osteoarthritis of the hip is a degenerative type of arthritis that occurs most often in middle-aged people and older. This disease causes the cartilage in the hip joint to wear away gradually over time. As the cartilage wears away, it becomes frayed and rough, causing the protective space between the bones in the joint to shrink. As the space in the joint shrinks, the bones begin to rub against each other, resulting in pain and other unpleasant symptoms.
Additionally, to make up for the lost cartilage, the damaged bones may start to grow outward and form bone spurs (known as osteophytes).
There is no single specific cause of osteoarthritis of the hip. Still, several factors may increase your likelihood of developing the disease, including:
- Age.
- Obesity.
- Family history of osteoarthritis.
- Improper formation of the hip joint at birth.
- Previous injury to the hip joint.

SYMPTOMS
There are several symptoms associated with osteoarthritis of the hip. These symptoms include:
- Pain around the hip joint that either worsens slowly over time or appears instantly.
- Pain in your groin or thigh that radiates to your buttocks or your knee.
- Pain that flares up with vigorous activity.
- Stiffness in the hip joint that makes walking or moving difficult.
- “Locking” or “sticking” of the joint or a grinding noise when you move caused by loose fragments of cartilage and other tissue interfering with the smooth motion of the hip.
- Decreased range of motion that affects the ability to walk and may cause a limp.
- Increased joint pain with rainy weather.

DIAGNOSIS
Your Florida Orthopaedic Institute physician will talk with you about your symptoms, medical history, and overall health, followed by a physical examination and imaging tests.
During the physical examination, your physician will look for:
- Pain when pressure is placed on the hip.
- Any problems with the way you walk (your gait).
- Signs of injury to the muscles, tendons, and ligaments surrounding the hip.
- Tenderness in and around the hip.
- Decreased range of hip motion.
- A grating sensation inside the joint during movement.
The initial imaging test your physician will order is an x-ray. X-rays create detailed pictures of dense structures, such as bones. This test will show if your hip joint space has narrowed and any other changes in the bone. It can also indicate the formation of any bone spurs. Occasionally, a magnetic resonance imaging (MRI) scan, a computed tomography (CT) scan, or a bone scan may be needed to better determine the condition of the bone and soft tissues of your hip. These tests are not typically ordered but are available.
TREATMENT OVERVIEW
Although there is no cure for osteoarthritis of the hip, there are several treatment options, both surgical and nonsurgical, that can help relieve pain and improve mobility. Your Florida Orthopaedic Institute physician will create a treatment plan suited for you and your needs.
NONSURGICAL TREATMENTS
There are many different nonsurgical treatments your physician may recommend, including:
- Lifestyle modifications. There are some changes you can make to your daily routine to help protect your hip joint and slow the progress of osteoarthritis. For example, you can minimize activities that aggravate the condition. These can include climbing stairs or switching from high impact activities like jogging or tennis to lower impact activities like swimming or cycling.
- Physical therapy. Specific exercises can help increase your range of motion and flexibility while also strengthening the muscles in your leg and hip. During physical therapy, you will perform individualized exercises that meet your needs and lifestyle.
- Assistive devices. Using walking supports like a crutch, cane, or walker can improve mobility and independence. Using assistive aids like a long-handled reacher to pick up low-lying things will help you avoid movements that may cause pain.
- Medications. If your pain affects your daily routine, your Florida Orthopaedic Institute physician may add one of the following medications to your treatment plan: Nonsteroidal anti-inflammatory drugs like Aleve (naproxen) and Advil (ibuprofen), cortisone (anti-inflammatory steroid) or Tylenol (acetaminophen, an over-the-counter pain reliever).
SURGICAL TREATMENT
If nonsurgical treatment is ineffective or if your pain and symptoms are severe, your physician may recommend a surgical procedure. There are several different surgical treatments your physician may choose for you, such as:
- Osteotomy. A procedure that takes the pressure off the hip joint by cutting and realigning the head of the thighbone or the socket.
- Hip resurfacing. The damaged bone and cartilage in the hip socket (acetabulum) are removed and replaced with the metal shell. Then the head of the femur is capped with a smooth metal covering.
- Total hip replacement. During this procedure, both the damaged acetabulum and femoral head are removed and replaced by either a new metal, plastic, or ceramic joint.
Regardless of which surgical procedure is chosen, it takes some time to recover. During your recovery period, you will need physical therapy to regain strength and restore your range of motion. After your procedure, you may need to use a cane, crutches, or a walker for a short time. In most cases, surgery relieves the pain of osteoarthritis and makes it possible to perform daily activities more easily.
NEXT STEPS
Talk to your Florida Orthopaedic Institute physician to learn more about osteoarthritis of the hip.
Areas of Focus
- Hip & Thigh
- Avascular Necrosis (Osteonecrosis)
- Groin Strains and Pulls
- Hamstring Injuries
- Hip Arthroscopy
- Hip Dislocation
- Hip Flexor Strains
- Hip Fractures
- Hip Hemiarthroplasty
- Hip Impingement Labral Tears
- Hip Muscle Strains
- Hip Pointers and Trochanteric Bursitis
- Iliopsoas Tenotomy
- Labral Tears Of The Hip (Acetabular Labrum Tears)
- Osteoarthritis of the Hip
- Osteoporosis
- Bone Health Clinic
- Pelvic Ring Fractures
- Piriformis Syndrome
- Sports Hernias (Athletic Pubalgia)
- Thigh Fractures
- Thigh Muscle Strains
- Total Hip Arthroplasty
- Total Hip Replacement - Anterior Approach
The following Florida Orthopaedic Institute physicians specialize in Osteoarthritis of the Hip:
Specialties
- AC Joint Injuries
- Achilles Tendinitis - Achilles Insertional Calcific Tendinopathy (ACIT)
- Achilles Tendon Rupture
- Achilles Tendonitis
- ACL Injuries
- Ankle Fracture Surgery
- Ankle Fractures (Broken Ankle)
- Ankle Fusion Surgery
- Anterior Cervical Corpectomy & Discectomy
- Arthroscopic Articular Cartilage Repair
- Arthroscopic Chondroplasty
- Arthroscopic Debridement of the Elbow
- Arthroscopy Of the Ankle
- Articular Cartilage Restoration
- Artificial Disk Replacement (ADR)
- Aspiration of the Olecranon Bursa - Fluid In Elbow
- Atraumatic Shoulder Instability
- Avascular Necrosis (Osteonecrosis)
- Bankart Repair
- Basal Joint Surgery
- Bicep Tendon Tear
- Bicep Tenodesis
- Bone Cement Injection
- Bone Growth Stimulation
- Bone Health Clinic
- Broken Collarbone
- Bunions
- Bursitis of the Shoulder (Subacromial Bursitis)
- Calcific Tendinitis of the Shoulder
- Carpal Tunnel Syndrome
- Charcot Joint
- Chiropractic
- Clavicle Fractures
- Colles’ Fractures (Broken Wrist)
- Common Foot Fractures in Athletes
- Community Outreach
- Cubital Tunnel Syndrome
- De Quervain's Tenosynovitis
- Deep Thigh Bruising
- Degenerative Disk Disease
- Diffuse Idiopathic Skeletal Hyperostosis (DISH)
- Discectomy
- Discitis Treatment & Information
- Dislocated Shoulder
- Dupuytren’s Disease
- Elbow
- Elbow Bursitis
- Elbow Injuries & Inner Elbow Pain in Throwing Athletes
- Epidural Injections for Spinal Pain
- Finger Dislocation
- Flexor Tendonitis
- Foot Stress Fractures
- Foot, Ankle & Lower Leg
- Foraminotomy
- Fractured Fingers
- Fractures Of The Shoulder Blade (Scapula)
- Fractures Of The Tibial Spine
- Functional Nerve Transfers of The Hand
- Ganglion Cysts
- General Orthopedics
- Glenoid Labrum Tear
- Golfer's Elbow
- Groin Strains and Pulls
- Growth Plate Injuries Of The Elbow
- Hallux Rigidus Surgery - Cheilectomy
- Hammer Toe
- Hamstring Injuries
- Hand & Finger Replantation
- Hand & Wrist
- Hand Nerve Decompression
- Hand Skin Grafts
- Hand, Wrist, Elbow & Shoulder
- Heat Injury/Heat Prostration
- High Ankle Sprain (Syndesmosis Ligament Injury)
- Hip & Thigh
- Hip Arthroscopy
- Hip Dislocation
- Hip Flexor Strains
- Hip Fractures
- Hip Hemiarthroplasty
- Hip Impingement Labral Tears
- Hip Muscle Strains
- Hip Pointers and Trochanteric Bursitis
- Hyperextension Injury of the Elbow
- Iliopsoas Tenotomy
- Iliotibial Band Syndrome
- Impingement Syndrome of the Shoulder
- Interlaminar Implants
- Interlaminar Lumbar Instrumental Fusion: ILIF
- Interventional Pain Management
- Interventional Spine
- Intraarticular Calcaneal Fracture
- Joint Replacement
- Knee & Leg
- Kyphoplasty (Balloon Vertebroplasty)
- Kyphosis
- Labral Tears Of The Hip (Acetabular Labrum Tears)
- Laminectomy: Decompression Surgery
- Lateral Collateral Ligament (LCL) Injuries
- Lisfranc Injuries
- Little League Shoulder
- LITTLE LEAGUER'S ELBOW (MEDIAL APOPHYSITIS)
- Lumbar Epidural Steroid Injection
- Lumbar Interbody Fusion (IBF)
- MACI
- Mallet, Hammer & Claw Toes
- Medial Collateral Ligament Injuries
- Meniscus Tears
- Metatarsalgia
- Minimally Invasive Spine Surgery
- Morton’s Neuroma
- Muscle Spasms
- Muscle Strains of The Calf
- Nerve Pain
- Neuromas (Foot)
- Neurosurgery
- Olecranon Stress Fractures
- Orthopaedic Total Wellness
- Orthopaedic Trauma
- Orthopedic Physician Or A Podiatrist? Definition of a Podiatrist
- Osteoarthritis of the Hip
- Osteoporosis
- Outpatient Spine Surgery
- Partial Knee Replacement
- Patellar Fracture
- Pelvic Ring Fractures
- Peripheral Nerve Surgery (Hand) Revision
- Pinched Nerve
- Piriformis Syndrome
- Piriformis Syndrome
- Plantar Fasciitis
- Plastic Surgery
- Podiatry
- Primary Care Sports Medicine
- Quadriceps Tendon Tear
- Radial Tunnel Syndrome (Entrapment of the Radial Nerve)
- Revascularization of the Hand
- Reverse Total Shoulder Replacement
- Rheumatoid Arthritis (RA) of the Shoulder
- Rheumatoid Arthritis Of The Hand
- Robotics
- Rotator Cuff Tears
- Runner's Knee
- Sacroiliac Joint Pain
- Sciatica
- Scoliosis
- Senior Strong
- Shin Splints
- Shoulder
- Shoulder Arthritis
- Shoulder Arthroscopy
- Shoulder Injury: Pain In The Overhead Athlete
- Shoulder Replacement
- Shoulder Separations
- Shoulder Socket Fracture (Glenoid Fracture)
- SLAP Tears & Repairs
- Spinal Fusion
- Spine
- Spondylolisthesis and Spondylolysis
- Sports Foot Injuries
- Sports Hernias (Athletic Pubalgia)
- Sports Medicine
- Sports Wrist and Hand Injuries
- Sprained Ankle
- Sprained Wrist Symptoms and Treatment
- Subacromial Decompression
- Sudden (Acute) Finger, Hand & Wrist Injuries
- Targeted Muscle Reinnervation (TMR)
- Tendon Transfers of The Hand
- Tennis Elbow Treatment
- Thigh Fractures
- Thigh Muscle Strains
- Thumb Ulnar Collateral Ligament Injuries
- Total Ankle Replacement
- Total Hip Arthroplasty
- Total Hip Replacement - Anterior Approach
- Total Knee Replacement Surgery
- Trapezius Strain (Muscle Strain of The Upper Back)
- Traumatic Shoulder Instability
- Tricep Pain & Tendonitis
- Trigger Finger
- Turf Toe
- UCL (Ulnar Collateral Ligament) Injuries
- Ulnar Neuritis
- Valgus Extension Overload
- Vertebroplasty
- WALANT (Wide Awake Local Anesthesia No Tourniquet)
- Whiplash and Whiplash Associated Disorder (WAD)
- Wound Care
- Wrist Arthroscopy
- Wrist Fractures
- Wrist Tendonitis
Services
- Physical Medicine & Rehabilitation
- Physical Therapy
- Primary Care Sports Medicine
- PROMs (Patient-Reported Outcome Measures)
- Same-Day Orthopaedic Appointments Now Available
- Sports Medicine
- Sports-Related Concussion Treatment
- Telehealth Page
- Telemedicine
- Workers' Compensation
- Workers' Compensation Dispensary
- X-Ray
