
By: Katheryne (Kat) Downes, Ph.D., MPH
Director of Health Research, Outcomes & Evaluation
Florida Orthopaedic Institute
NOTE: This post is not a substitute or replacement for professional medical advice. If you have any questions about your medical condition or treatment, please seek your doctor’s advice.
You might be reading this post because you (or a loved one) are thinking about having a joint replaced and wondering whether your current weight will be a problem.
Or maybe you were just told that you need to lose weight before you can get a joint replaced.
Whatever brought you here today- Welcome to FOI’s Bones of the Bay Blog! Here we discuss important medical topics in easy-to-understand language to help patients learn more about their health and healthcare.
Today’s post is all about the role of weight in deciding to have joint replacement surgery and the impact your weight can have on your recovery from surgery. In Part 1, we will talk about what numbers a doctor looks at to evaluate your possible risks, why those numbers are used, and why your weight matters more broadly. In Part 2, we sit down with Dr. Michael Miranda to talk about how he thinks about a patient’s weight when making decisions about whether to operate and his advice for patients who may be struggling with this issue.
So, let us start with the basics.
How does your doctor look at your weight?
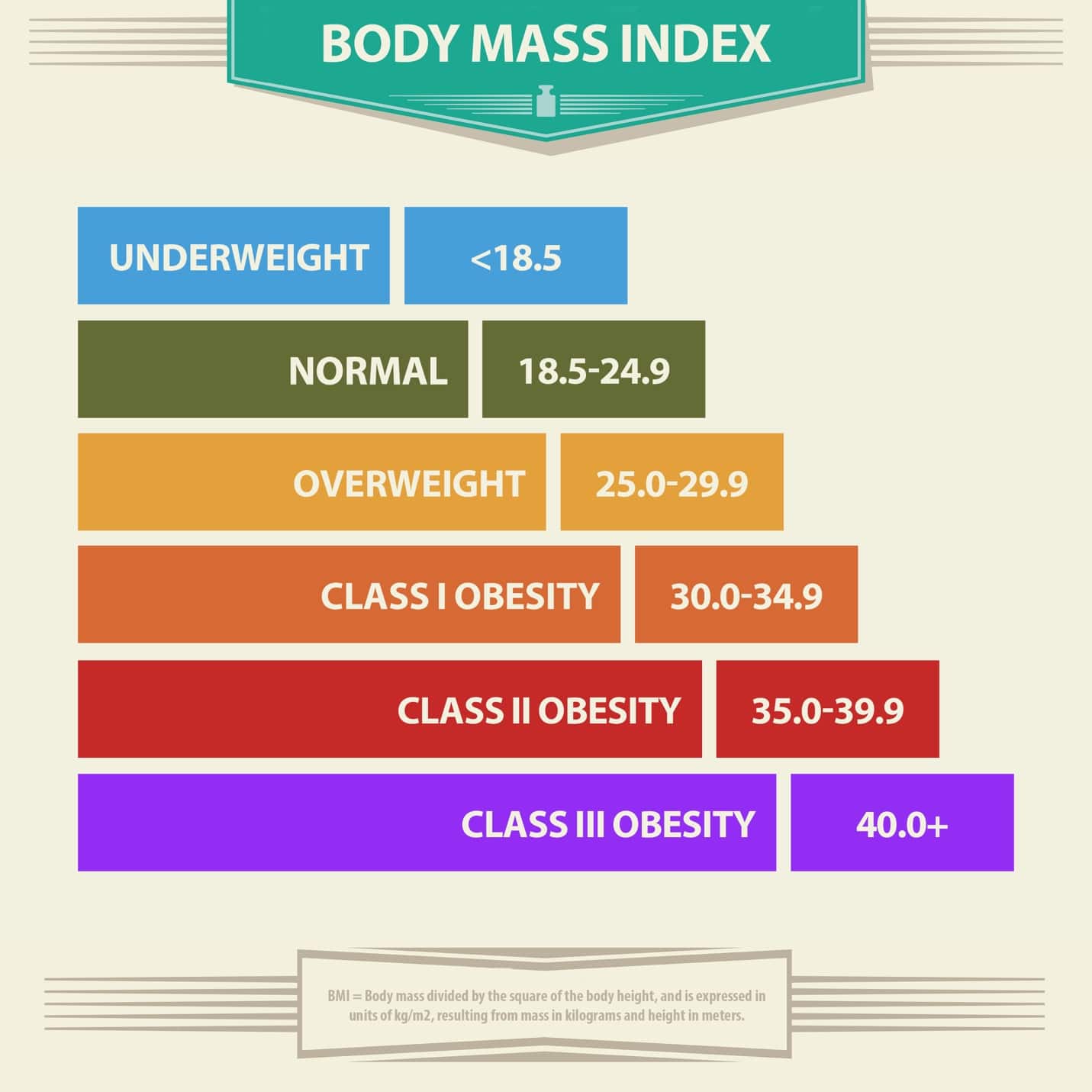
When you see most doctors, they usually have you step on a scale to record your weight and ask you for (or measure) your height. They can calculate your Body Mass Index (or BMI, for short) with these two numbers. The BMI is used as a general health screening tool, the same way that taking your temperature and blood pressure are used to watch other parts of your health.
You can use this free BMI calculator from the CDC website to determine your BMI right now.
Once your doctor has this number, they compare it to a chart like this to figure out what category your weight is in:
If you just found out that your BMI is above the “healthy” category- you are not alone:
The United States is in an ‘obesity epidemic’ because almost half of the country (42.4%) now has a BMI of 30+, and this number has been rising year after year. (1)

Where did BMI categories come from?
The categories are based on studies that looked at people with different BMIs and how often they were getting different diseases. We have learned that the risks start going up when you have a BMI that is 25 or higher. But the risks increase a lot when you have a BMI of 30 or higher, which is classified as “obesity.” (2-3)
According to the CDC (2-3), obesity increases the risk of Death, Gallbladder disease, Heart blockages, High blood pressure, Osteoarthritis, Stroke, High cholesterol, Sleep apnea, Body pain, Type 2 Diabetes, Some cancers, Chronic inflammation.
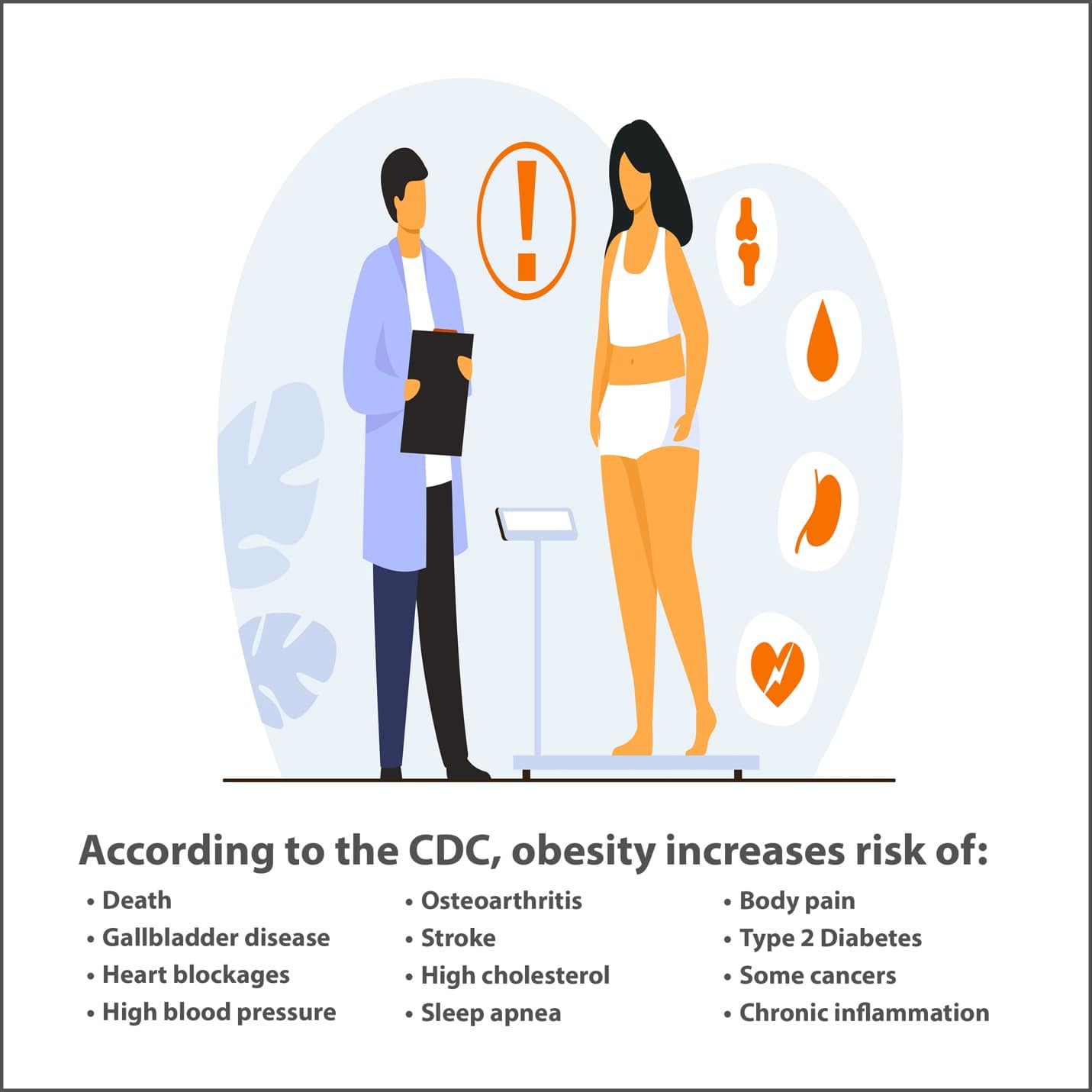
*Obesity has also been shown to increase the risk of severe illness with COVID-19 infection. (4)
The risks of all the above diseases tend to increase more as the BMI goes higher. So, risks are higher for BMIs in Class II vs. Class I and higher for Class III vs. Class II.
The fact that almost half of the country is now obese means that our health risks are generally going up as a nation. Not surprisingly, it also means that healthcare costs are going up.
What causes obesity?
You might be tempted to think that the answer is just: eating too much and exercising too little.
The truth is that it is a lot more complicated than that…
Yes, the number of calories you eat daily, minus the amount you burned off will generally determine whether you are losing or gaining weight (or holding steady). But what determines how many calories you eat and how much you burn off each day?
There are a few great resources for this (5-6), but here is a quick summary:
Environment & Behavior:
Do you have access to healthy food? Or do you live in a ‘food desert’, where healthy food is far away, and the nearest food is very bad for you? (junk food, candy, etc.).
Do you have a safe place nearby to walk/exercise?
Is your pantry or fridge stocked with mostly unhealthy options? (It’s harder to make healthy decisions if you are surrounded by junk food!)
Do you tend to go out to eat with friends and family often? If so, peer pressure (both obvious and not so obvious) can make you eat more food than if you were alone. (7)
Do you have a job that has you sitting for 8 hours a day at a desk? That is called a “sedentary” job, and it’s also not good for you! (8)
Genetics:
There is some early evidence that certain people do have genetics that make it easier for them to gain weight and harder to lose weight.
Other diseases and medications:
Certain diseases, like polycystic ovary syndrome (PCOS) and hypothyroidism (where your thyroid is under-performing), are associated with weight gain. Certain medications can also result in weight gain.
Stress & sleep:
Stress has both direct and indirect effects on our bodies. Being stressed for a long time (chronic stress) exposes us to certain hormones (like cortisol), which can harm us if we have high levels for too long. It can throw your body’s function out of whack: it can result in system-wide inflammation and pain. (9)
Indirectly, many people also tend to eat more and sleep less when they are stressed out. Not getting enough sleep can also throw our body “off” and lead to weight gain.
The mind-body connection:
There is also a complex mind-body connection around food, hunger, and feeling full (called “satiety,” pronounced “SAY-shuh-tee”). Some signals happen when we chew and when our stomach stretches from the food going into it. But there is a time delay- it’s not instant. We are supposed to have signals that bounce back to say: “We’re full – don’t eat any more.” For some people, this system doesn’t work correctly. Therefore, they can feel hungry when they aren’t, and might not feel full even though they are stuffed! (10-11)
Eating for comfort and for pleasure is also definitely a thing! (12)
Knowledge about nutrition and exercise:
Did your parents teach you what a healthy portion size is? Did they tell you how many glasses of water you should be drinking daily? Did they teach you about calorie density? Did they teach you how to read a nutritional label on food?
Mine didn’t. And I would guess that most of you didn’t get that information from your family either. And it wasn’t because they didn’t want us to know- it was because they also weren’t taught these healthy habits! Yet, it is incredibly important for being truly healthy.
Did you know that the average American portion served in a restaurant is generally 2-3x the size it used to be? (13) And it’s not just the amount of food that is piled on the plate- it is the size of the food itself. For example, 20 years ago, the average cheeseburger was 4.5oz… today, it is 8oz! This is why there has been a push toward showing calorie information on restaurant menus and making nutrition labels easier to read. (13)
I was personally horrified when I learned how many calories were in one of my favorite frozen dessert treats! The same thing happened with some of my favorite meals at certain restaurants. In some cases, it’s the entire days’ worth of calories (or sometimes 2-3x that amount!).
So, this is all to say that there are a lot of different reasons why so many of us are struggling with our weight, but there are definitely some great options out there to help you make the changes if you want to be healthier.
Okay, so now I know a lot more about why obesity happens and the health risks, but what does this have to do with joint replacement surgery?
In addition to increasing the risk of developing other diseases, obesity has also been shown to increase the risk of certain outcomes during and after surgery:
- Increased use of pain medication after surgery. (14)
- Having to stay overnight at the hospital when you were supposed to be discharged the same day. (15)
- Longer surgery time. (16-17)
- Surgical complications. (16)
- Longer hospital length of stay (17-18)
- Needing additional surgeries. (reoperation) (19)
- Being re-admitted to the hospital due to a problem specifically with your joint replacement. (19)
- Surgical site infection. (19)
- Infection of the replaced joint. (called ‘periprosthetic infection’) (20)
In short, your doctor is worried about your weight because a too-high BMI can put you in danger during surgery and make your recovery more difficult.
In Part II of this post, I sat down with Dr. Michael Miranda to talk about how he thinks about weight and total joint surgery.
Click here to read our conversation.
Subscribe to this Blog: Email us and put “SUBSCRIBE” in the subject line.
Questions? Suggestions for a future topic? Click here to email us at Bones of the Bay.
References:
- CDC Obesity Data.
- CDC on Adult BMI.
- CDC on Health Effects of Overweight and Obesity.
- CDC on Obesity and COVID-19
- Obesity and Overweight Causes from NICHD – NIH.
- CDC on Obesity in Adults.
- Health Essentials Article on Peer Pressure and Healthy Eating.
- Stamatakis E, Gale J, Bauman A, Ekelund U, Hamer M, Ding D. Sitting Time, Physical Activity, and Risk of Mortality in Adults [published correction appears in J Am Coll Cardiol. 2019 Jun 4;73(21):2789]. J Am Coll Cardiol. 2019;73(16):2062-2072. doi:10.1016/j.jacc.2019.02.031
- Hannibal KE, Bishop MD. Chronic stress, cortisol dysfunction, and pain: a psychoneuroendocrine rationale for stress management in pain rehabilitation. Phys Ther. 2014;94(12):1816-1825. doi:10.2522/ptj.20130597<
- Miquel-Kergoat S, Azais-Braesco V, Burton-Freeman B, Hetherington MM. Effects of chewing on appetite, food intake and gut hormones: A systematic review and meta-analysis. Physiol Behav. 2015;151:88-96. doi:10.1016/j.physbeh.2015.07.017
- Murphy KG, Bloom SR. Gut hormones and the regulation of energy homeostasis. Nature. 2006;444(7121):854-859. doi:10.1038/nature05484
- Kringelbach ML, Stein A, van Hartevelt TJ. The functional human neuroanatomy of food pleasure cycles. Physiol Behav. 2012;106(3):307-316. doi:10.1016/j.physbeh.2012.03.023
- We Can!® Community News Feature
- Rajamäki TJ, Puolakka PA, Hietaharju A, Moilanen T, Jämsen E. Predictors of the use of analgesic drugs 1 year after joint replacement: a single-center analysis of 13,000 hip and knee replacements. Arthritis Res Ther. 2020;22(1):89. Published 2020 Apr 21. doi:10.1186/s13075-020-02184-1
- Crawford DA, Hurst JM, Morris MJ, Hobbs GR, Lombardi AV Jr, Berend KR. Impact of Morbid Obesity on Overnight Stay and Early Complications With Outpatient Arthroplasty. J Arthroplasty. 2020;35(9):2418-2422. doi:10.1016/j.arth.2020.04.098
- Hartford JM, Graw BP, Frosch DL. Perioperative Complications Stratified by Body Mass Index for the Direct Anterior Approach to Total Hip Arthroplasty. J Arthroplasty. 2020;35(9):2652-2657. doi:10.1016/j.arth.2020.04.018
- Tompkins G, Neighorn C, Li HF, et al. Extremes of body mass index have significant impact on complications, readmissions, and utilization of post-acute services after primary total hip arthroplasty. Bone Joint J. 2020;102-B(7_Supple_B):62-70. doi:10.1302/0301-620X.102B7.BJJ-2019-1527.R1
- Mohamed NS, Wilkie WA, Remily EA, et al. The Rise of Obesity among Total Knee Arthroplasty Patients [published online ahead of print, 2020 May 22]. J Knee Surg. 2020;10.1055/s-0040-1710566. doi:10.1055/s-0040-1710566
- Heo SM, Harris I, Naylor J, Lewin AM. Complications to 6 months following total hip or knee arthroplasty: observations from an Australian clinical outcomes registry. BMC Musculoskelet Disord. 2020;21(1):602. Published 2020 Sep 10. doi:10.1186/s12891-020-03612-8
- Shearer J, Agius L, Burke N, Rahardja R, Young SW. BMI is a Better Predictor of Periprosthetic Joint Infection Risk Than Local Measures of Adipose Tissue After TKA. J Arthroplasty. 2020;35(6S):S313-S318. doi:10.1016/j.arth.2020.01.048
